Hello. Welcome to the Mosaic Diagnostics Blog. My name is Jessica Bonovich, RN, BSN. I’m the nurse consultant here at Mosaic Diagnostics. Today I’m going to be discussing oxalates, which are one of the many things that are tested for in the Organic Acids Test (OAT). Oxalates are of particular interest to patients who have pain and in non-verbal children with behavioral issues. Frequently, these individuals are experiencing pain as the result of oxalate crystals precipitating with minerals in tissue, including the formation of kidney stones. The Organic Acid Test is well suited to determine if this is likely occurring. When determining the best course of action we look at the proportion of the oxalate, the metabolite of oxalate, and the patient’s symptoms.
As the nurse consultant at the lab, it is my primary job to review test results with people. and as a result, I see a lot of Organic Acids Tests. Doctors and patients are often surprised to learn that Candida and Aspergillus species can produce oxalates. These species have certain enzymes that allow them to use glyoxalate as a means of making energy (it is an intermediate in their TCA cycle). Individuals with elevations in Candida or Aspergillus frequently have a subsequent elevation in oxalate metabolites. The degree of elevation may or may not be proportional to the yeast/mold overgrowth and this is an important distinction when evaluating the significance of the markers. If the elevation is proportional, I can easily point toward yeast as the culprit. If the oxalates are disproportional, it can be related to several other factors.
To some extent, all individuals will obtain oxalates from three sources: liver cells (endogenously), yeast species (exogenously), and food (also exogenous). The reference ranges on our test show the typical accumulation of oxalate metabolites from all three sources.
In humans and in yeast, glyoxalate is the parent compound that can be converted into the three metabolites measured on the Organic Acids Test (OAT): glyceric, glycolic, and oxalic acid (Figure 1).
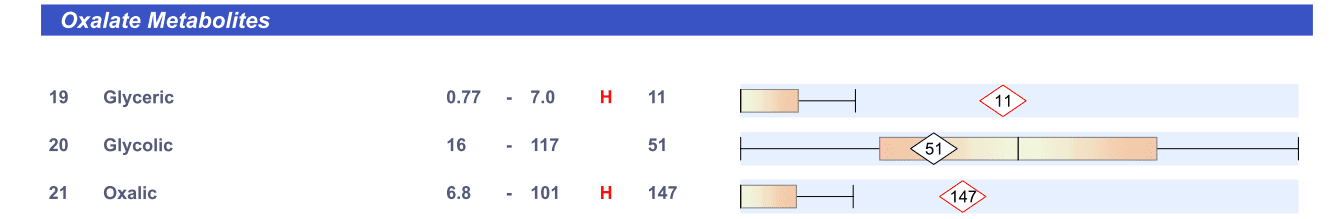
It can also be converted into glycine which is not measured on the OAT. Individuals with primary, secondary, or tertiary hyperoxaluria have genetic deficiencies in the enzymes that drive these pathways and cause the distinguishing features of the disease. People who are predisposed to stone formation may or may not have deficiencies in these enzymes. The degree to which a person will favor each pathway depends on a number of metabolic factors (including available precursor and pH of the cell). Elevations in all three metabolites can occur because of yeast and endogenous production. Food and Aspergillus on the other hand, produce oxalate in the body directly. So, when these are the source of excess, only oxalate will be elevated on the test.
Patient symptoms are a key component to all of this. It almost goes without saying that we treat the patient and not the number. Low oxalate values do not rule out an oxalate issue and extremely elevated values are not always equated with pain (though the potential certainly exists).
Let’s get back to the disproportional oxalate scenario. If a patient has mildly elevated yeast and moderately to highly elevated oxalate, what do you think would be the most likely cause?
a. Endogenous production
b. Yeast
c. Food
d. A combination of b. and c.
The correct answer is d. Food is a direct source of oxalate and the most common cause of disproportionately elevated oxalates. Yeast is contributing to the oxalates in this scenario but is not likely to be the only cause of the elevation. Patients like these should introduce calcium and magnesium supplementation with meals to help bind up excessive oxalates in the food (so they can be eliminated in stool). Many conventional doctors falsely believe that calcium supplementation should be avoided when oxalate stones are a problem. They forget that calcium levels are maintained at precise levels in the blood no matter what the intake is. This is because without calcium, the heart will not pump. So, several mechanisms are in place to ensure adequate levels are maintained at all times. Avoiding calcium is only likely to increase osteopenia and not at all likely to reduce stone formation.
Let’s walk through another scenario. An individual presents with extreme pain in the muscles and history of stone formation. The patient has very elevated Candida and eats a high oxalate diet. All of the oxalate metabolites on the OAT are normal. What is the most likely scenario?
a. Oxalates are not a problem
b. Endogenous production
c. Food and yeast are not a problem
d. None of the above
The correct answer is d. This is a scenario that I refer to as hidden oxalate toxicity. This patient should have elevated oxalate metabolites. Based on their history and lab results, oxalates would be expected. It is likely that oxalates are present in the body. However, they are precipitating in tissues before they ever make it into the urine. These patients are usually the most extreme cases of pain. They are also the people who do very well once all of the sources of oxalate have been eliminated. It is important to remember that when patients are in pain, removing oxalates should be done SLOWLY. Otherwise the patients are likely to experience an increase in pain as a result of “oxalate dumping”. When oxalate crystals are already in the tissues, mobilizing them can cause irritation. I recommend that patient introduce therapies one at a time, thoughtfully, over several weeks to months.
Okay, last one. This is a patient with moderately high yeast metabolites, a diet rich in fruits and veggies, and severely elevated oxalate metabolites. To give this some perspective, the reference range for oxalates is 100 mmol/mol. This patient has close to 1000. The patient has symptoms of yeast overgrowth and fatigue as the chief complaints. What is the most likely cause of the extremely elevated oxalates?
a. Yeast
b. Diet
c. Endogenous production
d. All of the above
If your answer was d, you are correct. This patient has disproportional oxalates beyond what would be expected in diet. The patient certainly has the potential to accumulate oxalates in the tissues. However, since she is eliminating it effectively, it is not causing her pain at this time. Measures should still be taken to decrease the oxalate burden. We have much more to learn about the tendency for a person to form oxalate crystals. Several genes (AGXT, GRPHR, and HOGA1) have been implicated (all of which are identified on the GPL SNP1000 test). Even if these genes are not mutated, some individuals still have a tendency toward oxalate stone formation. The high glyoxalate production is only one factor.
Remediation of high oxalates is a multi-step process. Elimination of yeast is always important and not only because of excessive production. Pathogenic yeast can also cause an imbalance in beneficial bacteria that help to degrade oxalates. Many studies have demonstrated that oxalobacter can reduce oxalate stone formation (hence the name). As of right now, testing for oxalobacter is available primarily in research settings and supplements are not widely available to the public (though I expect that they will be soon). Fortunately, there are other beneficial bacteria species shown to reduce oxalic acid. Many of these are already available probiotic form. These include Lactobacillus acidophilus, Lactobacillus casei, Bifidobacterium breve, and Bifidobacterium lactis all of which are available in Lactoprime and Ther-biotic Complete probiotic formulas.
Awareness of oxalates in food and elimination of those foods highest in oxalate (like spinach, soy, almonds, sweet potatoes, and raspberries) is important. Keep in mind that a low oxalate diet should only be done with the help of a practitioner and only when there is a clear need. The foods that contain oxalate are healthy and provide many nutrients that our bodies need to maintain healthy homeostasis. People forget that the oxalate content alone is not the only factor in oxalate absorption. The oxalate to calcium/magnesium ratio should be taken into account when we consider the potential for oxalate accumulation. If a food has equal amounts of both calcium and oxalate, it is likely that neither one will be absorbed very well. Plenty of bile acid needs to be available to prevent fats from binding with calcium. Both taurine and glycine strengthen bile acid but glycine increases oxalate. Glycine is where our endogenous production of glyoxalate starts. Keep this in mind when you are choosing supplements.
Lastly, sufficient B6 is required to help with the conversion of glyoxalate to glycine in the body. Maintaining sufficient levels of vitamin B6 will help with the endogenous production. However, the active form (P5P) is poorly absorbed. I recommend that patients in pain start with low doses of pyridoxine hydrochloride (10 mg) and work up to higher doses as tolerated. The upper limit is 100 mg per day. Patients without pain can usually safely start at 50 mg per day.
Wow, so that was a lot. Oxalates are a topic of much interest in our patient population so I want to be as thorough as possible. If in doubt, call the lab and speak with a consultant. We have lots of experience looking at tests results and can provide insight into the patterns that are occurring on the results.
Test Oxalates with the Organic Acids Test
Evaluation of Oxalates and other downstream metabolites from various metabolic pathways provides insight into important areas related to gut health, mitochondrial dysfunction, neurotransmitter status, indicators of detoxification and macronutrient breakdown and nutritional status.
The Organic Acids Test (OAT) provides a comprehensive nutritional and metabolic snapshot of an individual’s overall health. The OAT measures 76 organic acids from one easy to collect urine sample.
More Oxalate Related Resources
REFERENCES:
Finkielstein, V., Goldfarb, D., (2006). Strategies for preventing calcium oxalate stones. Canadian Medical Association Journal , 174 (100). Published online doi: 10.1503/cmaj.051517
Herb, Nutrient, and Drug Interactions. (1st edition). (2008). St. Louis, MO, Mosby, Elsevier
Liebman, M., Costa, G. (2000). Effects of calcium and magnesium on urinary oxalate excretion after oxalate loads. Journal of Urology, 163(5): 1565-1659.
Matkovic, V., Heaney, R.P., (1992). Calcium balance during human growth: evidence for threshold behavior. The American Society for Clinical Nutrition, 55(5): 992-996.
Pennistion, K., Nakada, S. (2009). Effect of Dietary Changes on Urinary Oxalate Excretion and Calcium Oxalate Supersaturation in Patients With Hyperoxaluric Stone Formation. Urology, 73(3):484-489.
Physicians Desk Reference for Nutritional Supplements. (2nd edition). (2008). Montvale, NJ: Thomson PDR
Rushton, HG., Spector, M. (1982). Effects of magnesium deficiency on intratublar calcium formation and crystalluria in hyperoxaluric rats. Journal of Urology, 127(3): 598-604.
Poore, R.E., Hurst, C.H., Assimos, D.G., Holmes, R.P. (1997). Pathways of hepatic oxalate synthesis and their regulation. Cell Physiology. 272(1), C289-C294
Shaw, W. (2009). Autism: Beyond the Basics. Self Published, USA.
Weaver, C. (1994). Age related calcium requirements due to changes in absorption and utilization. Journal of Nutrition, 124(8): 1418S-1425S.