An elimination diet is designed to help identify and address food sensitivities by temporarily removing certain foods from the diet based on clinical presentation and IgG Food MAP results. The diet typically lasts 2 to 3 months and consists of 4 Pillars – Prepare, Eliminate, Restore, and Reintroduce – each essential for guiding patients through the process.
Before beginning an elimination diet, it is important to evaluate the patient’s clinical presentation alongside their IgG Food MAP results. These factors help identify which specific food(s) should be temporarily removed from their diet to address potential sensitivities. The duration of an elimination diet typically ranges from 2 to 3 months, depending on the patient’s individual response and symptom improvement. Setting a clear start and end date in collaboration with your patient is crucial for maintaining consistency and ensuring they receive adequate support throughout the process.
Once a start date has been established, proper preparation is key to the success of an elimination diet. This phase focuses on setting up routines and strategies that will help ensure compliance and optimize outcomes during the elimination and reintroduction stages.
Tracking Symptoms
Encourage patients to begin tracking their symptoms even before starting to eliminate foods. Recording digestive issues, skin changes, energy levels, mood, and other physical responses on a daily basis will help them recognize patterns. This symptom-tracking will become crucial during the reintroduction when assessing the impact of specific foods. A food journal or tracking app is recommended to ensure consistency.
Meal Planning and Adequate Nutrition
Planning meals ahead of time is very helpful during the elimination to avoid accidentally consuming reactive foods. Encourage patients to create weekly meal plans that include a variety of nutrient-dense foods while ensuring they meet their caloric and nutritional needs. Eliminating multiple foods can sometimes lead to inadequate caloric intake, so it’s important to ensure the diet remains balanced and rich in protein, healthy fats, fiber, vitamins, and minerals.
Choosing Organic When Possible
To minimize exposure to pesticides and other environmental toxicants that can exacerbate food sensitivities, it is recommend that patients choose organic options whenever possible, especially for the EWG’s “Dirty Dozen” list of produce. This step can help reduce the overall toxic burden on the body while the immune system is resetting during the elimination.
Staying Hydrated & Getting Adequate Rest
Remind patients of the importance of staying hydrated throughout the elimination process. Proper hydration supports digestion, nutrient absorption, regular bowel movements and detoxification pathways. Additionally, encourage patients to get plenty of rest, as quality sleep is essential for supporting digestion, immune system function, and overall healing while making these drastic dietary changes. Together, hydration and rest will optimize the body’s ability to adjust and recover throughout the elimination diet.

Elimination is focused on removing specific foods from the diet based on the results of the IgG Food MAP. The goal is to eliminate potential triggers to allow the gut and immune system to calm and reset.
Eliminate Specific Foods
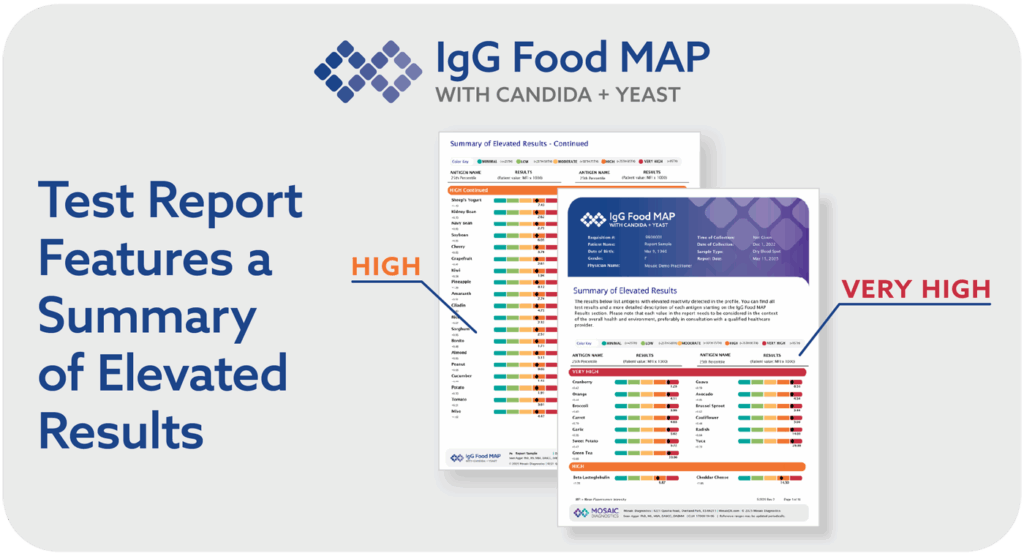
Patients should remove all foods that fall into the and Very High (>95th percentile) and High (75th-95th percentile) categories from their IgG Food MAP results. These foods are most likely to provoke immune reactions and should be avoided during elimination. Foods with Moderate sensitivity (50th-75th percentile) may also be considered for elimination, depending on the patient’s history and symptoms. Foods categorized as Low (25th-50th percentile) and Minimal (0-25th percentile) and are less likely to cause significant reactions but should still be monitored.
Eliminate Entire Food Groups (If Necessary)
In some cases, it may be beneficial to eliminate an entire food group rather than just individual foods. For example, if dairy shows multiple sensitivities across categories (e.g., milk, cheese, yogurt), eliminating all dairy products may be easier to adhere to, provide clearer results, and more relief during the elimination. Similarly, if multiple gluten-containing grains test positive, it might be advisable to adopt a completely gluten-free diet. This comprehensive approach can simplify the elimination process and reduce the risk of consuming hidden triggers.
By focusing on a clear elimination strategy tailored to the patient’s IgG Food MAP results, this phase lays the foundation for a successful reintroduction and long-term symptom management.
After eliminating foods identified by the IgG Food MAP food sensitivity test, the next critical step is to focus on restoring optimal gastrointestinal function. This involves the concepts of “Replace”, “Reinoculate”, and “Repair” to support digestive health and prepare the gut for the eventual reintroduction of foods.
Replace
In the context of an elimination diet, “replace” refers to replenishing essential digestive components that may be compromised, such as digestive enzymes, stomach acid (HCl), and bile acids. Many patients with food sensitivities may also experience inadequate digestion, which can exacerbate symptoms like bloating, gas, and malabsorption. Key replacement strategies include:
- Digestive Enzymes: Supplementing with a high-quality, broad-spectrum enzyme formula can support the proper and efficient breakdown of proteins, fats, and carbohydrates, alleviating some of the stress on the digestive system during the elimination.[1]
- HCl (Hydrochloric Acid): Individuals with low stomach acid (hypochlorhydria) may benefit from betaine HCl supplements to re-acidify the stomach, promote proper protein digestion and the absorption of essential nutrients. This re-acidification can enhance the activity of pepsin, a proteolytic enzyme, and potentially reduce the persistence of undigested foods that may trigger food sensitivities.[2],[3]
- Bile Acids: If bile production is low, some individuals may benefit from supplemental ox bile or bile salts to aid in the emulsification of dietary fats and promote the absorption of fatty acids and fat-soluble vitamins.[4],[5]
Reinoculate
Reinoculation with probiotics and prebiotics plays a significant role in alleviating food sensitivities by modulating the gut microbiota, enhancing immune tolerance, and improving overall digestive health:
- Probiotics: Reintroducing specific beneficial bacterial strains of Lactobacillus and Bifidobacterium species through a high-quality probiotic supplement supports the maintenance of gut integrity, provides antioxidant support, and promotes a healthy immune response.[6],[7],[8]
- Prebiotics: Prebiotic fibers, such as inulin and fructooligosaccharides (FOS), are essential for feeding beneficial bacteria. These fibers promote the growth of probiotics and can improve microbial diversity, which is key for long-term gut health.[9],[10]
Repair
Repair focuses on healing the gut lining to reduce inflammation and restore its barrier function, which may have been compromised by chronic food sensitivities and digestive dysfunction:
- L-Glutamine: This amino acid is essential for the regeneration of the intestinal lining and can help reduce symptoms of increased intestinal permeability.[11]
- Zinc Carnosine: This is a specific form of zinc that supports the mucosal lining and protects the gut lining.[12]
- Botanicals: Supplements derived from botanicals like curcumin from turmeric root, aloe vera, and slippery elm can promote a healthy inflammation response in the gut and soothe irritation.
- Essential Fatty Acids: Omega-3 fatty acids derived from fish oil have been shown to reduce inflammation and promote gut healing.[13]
- Vitamin D: Vitamin D supports gut healing by lowering inflammation, strengthening the intestinal barrier, and promoting beneficial gut bacteria.[14],[15]
By addressing digestive function, microbial balance, and mucosal repair, this stage sets the foundation for reintroducing foods.

Reintroduction is critical for identifying specific foods that still trigger sensitivities, and gradually expanding the patient’s diet after a period of elimination.[16] This process should be done methodically and can be based on the specific results provided by the IgG Food MAP or the patient’s preferences.
When reintroducing foods, it is important to test with the purest form of food available. For example, to test wheat, use a pure wheat cereal that contains only wheat. For dairy, test milk and different types of cheeses separately; however, yogurt, cottage cheese, and butter may not need to be tested separately. For eggs, test the whites and yolks separately using hard-boiled eggs.
Reintroduction Protocol
- Wait Period: After the elimination (typically lasting 2-3 months), foods should be reintroduced one at a time to accurately track any reactions. A new food can be reintroduced every 3 to 5 days, allowing time for potential delayed reactions, which may take up to 72 hours to appear.
- Order of Reintroduction Based on IgG Food MAP Results: The order specific foods are reintroduced in varies and should be agreed upon between the provider and the patient. Some methods to consider:
- Start with foods that were eliminated but had lower reactivity. For example, if all “Moderately” reactive foods were eliminated, starting with those may be preferred over starting with a “Very High” food.
- Start with the food the patient has had the hardest time not having in their diet. This can give the patient a little boost and help them remain compliant with reintroduction.
- Start with foods from categories where there were few reactions. For example, if the patient only reacted to one bean but reacted to 4 foods in the dairy category, it might be preferable to start with the bean over starting in the dairy category.
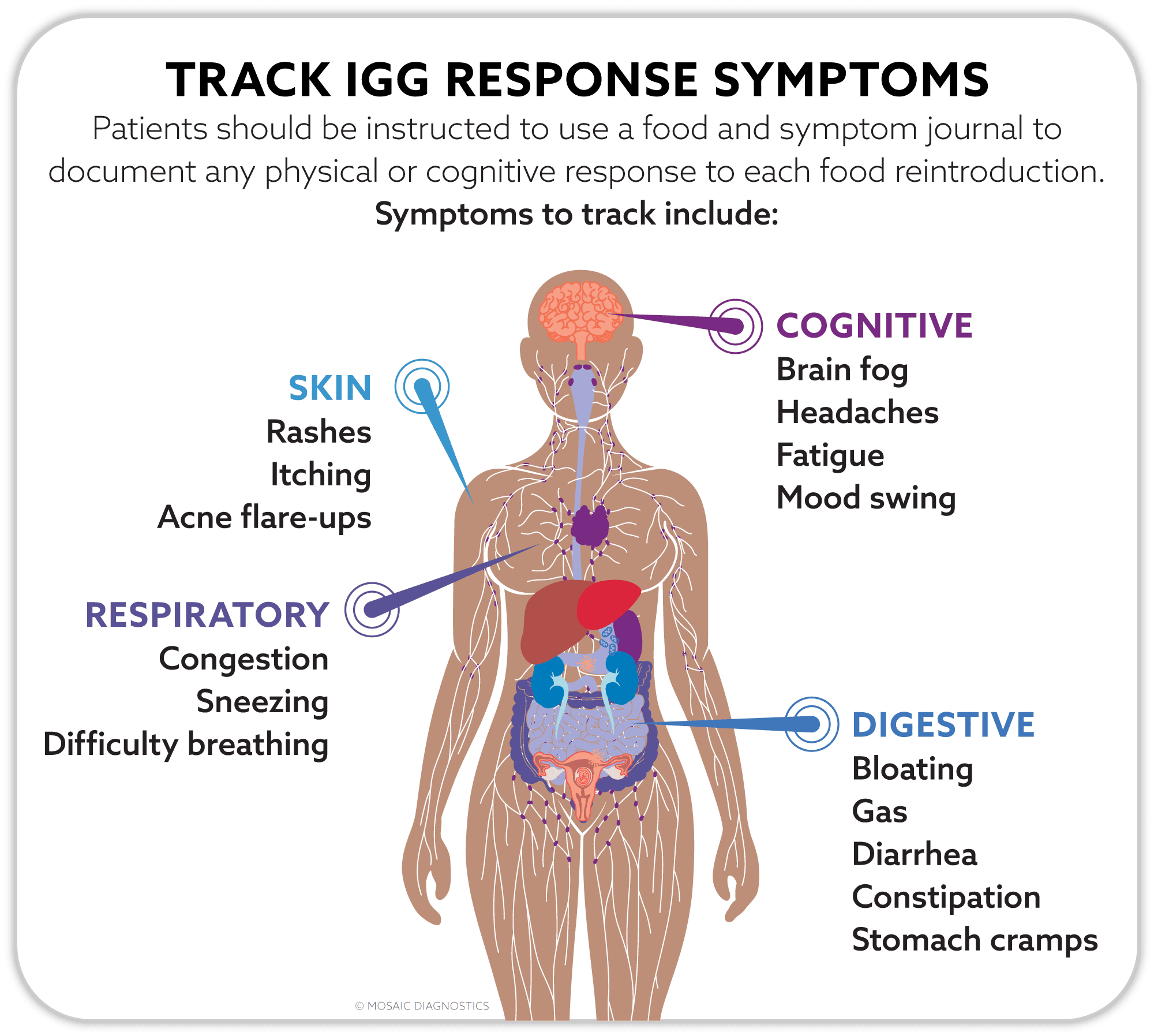
- Track Symptoms: Patients should be instructed to use a food and symptom journal to document any physical or cognitive response to each food reintroduction. Symptoms to track include:
- Digestive symptoms: bloating, gas, diarrhea, constipation, or stomach cramps.
- Skin reactions: rashes, itching, or acne flare-ups.
- Respiratory symptoms: congestion, sneezing, or difficulty breathing.
- Cognitive symptoms: brain fog, headaches, fatigue, or mood swings.
- Method of Reintroduction: For each reintroduced food, start with a small portion (a few bites) and wait 12-24 hours to see if any immediate reactions occur.
- If no symptoms arise, increase the portion size to a typical serving the following day and continue monitoring for another 12-24 hours. Continue this process for 3-5 full days.
- If symptoms develop, remove the food from the diet and wait for the symptoms to fully resolve (usually 2-3 days) before attempting another reintroduction.
- This food would be eliminated for another 2-3 months before attempting the reintroduction process with it again.
- If no symptoms occur, the food can be safely reintroduced into the regular diet.
- Common Patterns: Encourage individuals to watch for delayed or cumulative effects. Reactions may not be immediate but can build over several days of consumption. A detailed record of intake and symptoms will help identify such patterns.
IMPORTANT NOTE: Avoid reintroducing any foods that are known allergens. Before beginning the reintroduction of foods, it is important to review the signs and management of immediate hypersensitivity reactions with the patient. If they experience any immediate allergic reactions – such as swelling of face, mouth, or tongue; wheezing; or the appearance of rashes or hives – discontinue the food and seek medical attention immediately. Once the reaction is resolved, patients should seek provider guidance on how to safely proceed with the reintroduction process.
Need More Guidance?
For Practitioners Only
At MosaicDX, we prioritize your success in applying clinical insights provided by our testing. That’s why our clinical support team of medical doctors, naturopathic doctors, doctors of clinical nutrition, and registered dietitians, is here to assist you every step of the way.
With an active MosaicDX practitioner account, you gain access to one-on-one virtual consults with our clinical educators.
References
- Samadi N, Heiden D, Klems M, et al. Gastric Enzyme Supplementation Inhibits Food Allergy in a BALB/c Mouse Model. Nutrients. 2021;13(3):738. Published 2021 Feb 26. doi:10.3390/nu13030738
- Surofchy DD, et al. Food, Acid Supplementation and Drug Absorption – a Complicated Gastric Mix: a Randomized Control Trial. Pharm Res. 2019;36(11):155. doi:10.1007/s11095-019-2693-5
- Yago MR, et al. Gastric reacidification with betaine HCl in healthy volunteers with rabeprazole-induced hypochlorhydria. Mol Pharm. 2013;10(11):4032-4037. doi:10.1021/mp4003738
- Maldonado-Valderrama J, et al. The role of bile salts in digestion. Adv Colloid Interface Sci. 2011;165(1):36-46. doi:10.1016/j.cis.2010.12.002
- Macierzanka A, et al. Bile salts in digestion and transport of lipids. Adv Colloid Interface Sci. 2019;274:102045. doi:10.1016/j.cis.2019.102045
- Mazzocchi A, et al. The Role of Nutritional Aspects in Food Allergy: Prevention and Management. Nutrients. 2017;9(8):850. doi:10.3390/nu9080850
- Tian X, Liang X, He H, et al. Probiotics Alleviate Food Protein Allergy in Mice by Activating TLR4 Signaling Pathway. Mol Nutr Food Res. 2023;67(12):e2200579. doi:10.1002/mnfr.202200579
- Duan C, Ma L, Qin M, et al. Potential of Lactobacillus plantarum A56 in relieving food allergy through immunoregulation, antioxidation, and reshaping intestinal microbiota. J Nutr Biochem. 2024;125:109560. doi:10.1016/j.jnutbio.2023.109560
- Mazzocchi A, et al. The Role of Nutritional Aspects in Food Allergy: Prevention and Management. Nutrients. 2017;9(8):850. doi:10.3390/nu9080850
- Bai J, et al. Gut microbiota: A target for prebiotics and probiotics in the intervention and therapy of food allergy. Crit Rev Food Sci Nutr. 2024;64(11):3623-3637. doi:10.1080/10408398.2022.2133079
- Zuhl MN, et al. Effects of oral glutamine supplementation on exercise-induced gastrointestinal permeability and tight junction protein expression. J Appl Physiol (1985). 2014;116(2):183-191. doi:10.1152/japplphysiol.00646.2013
- Mazzocchi A, et al. The Role of Nutritional Aspects in Food Allergy: Prevention and Management. Nutrients. 2017;9(8):850. doi:10.3390/nu9080850
- Mazzocchi A, et al. The Role of Nutritional Aspects in Food Allergy: Prevention and Management. Nutrients. 2017;9(8):850. doi:10.3390/nu9080850
- Gargano D, et al. Food Allergy and Intolerance: A Narrative Review on Nutritional Concerns. Nutrients. 2021;13(5):1638. doi:10.3390/nu13051638
- Mazzocchi A, et al. The Role of Nutritional Aspects in Food Allergy: Prevention and Management. Nutrients. 2017;9(8):850. doi:10.3390/nu9080850
- Atkinson W, et al. Food elimination based on IgG antibodies in irritable bowel syndrome: a randomized controlled trial. Gut. 2004;53(10):1459-1464. doi:10.1136/gut.2003.037697