The material contained within this presentation is not intended to replace the services and/or medical advice of a licensed healthcare practitioner, nor is it meant to encourage diagnosis and treatment of disease. It is for educational purposes only. Any application of suggestions set forth in the following portions of this article is at the reader’s discretion and sole risk. Implementation or experimentation with any supplements, herbs, dietary changes, medications, and/or lifestyle changes, etc., is done so at your sole risk and responsibility. Views expressed are those of the presenter and not necessarily those of Mosaic Diagnostics.
Webinar Transcript
This is an automated AI transcript of the Webinar video seen above. For the most accurate account of Dr. Woeller’s presentation, please watch the webinar video on this page.
Well, hello everybody. This is Dr. Woeller here for Mosaic Edge, and we’re gonna talk about clostridia bacteria, autism and the organic acids test. I’m also gonna get into some new material here as well, and then I’m gonna show you where you can also follow me in addition to things that I do online for additional information, particularly on this topic and others as well.
So here’s the disclaimer, understanding that the information we’re discussing in this lecture is for educational purposes only. So I have been in clinical practice now for well over 25 years. I do a tremendous amount of speaking throughout the us also internationally, and I’ve been a clinical educator for formerly Great Plains Lab and now Mosaic Diagnostics. And then I’m also founder and clinical education director for an online academy called Integrative Medicine Academy, which has different courses for integrative and functional medicine practitioners.
I’m also the founder and education director for Autism Recovery System. And then in my own practice, I work a lot with individuals on the autism spectrum, but also patients with chronic and environmental health issues, gastrointestinal problems, autoimmune mold, mycotoxins, et cetera.
So we’re gonna break this down into a couple different sections, clostridia, organic acid test, and then autism, and then merge all of that information together. So let’s just start with Clostridia. We know it’s a, a, a major problem. Clostridia are a group of anaerobic bacteria that can inhabit the digestive system in us as humans. And there’s many types of clostridia bacteria that are actually non-pathogenic. So they could be normal inhabitants of the digestive system, but some of the species within this grouping are very problematic and can actually cause serious illness and even even death.
And so clostridium difficile is an example. There’s Clostridium botulinum tetanus as well, but those are relatively rare, fortunately. But the Clostridium difficile is not rare. In fact, the image you see here on your right is somebody with what’s called pseudo membranous colitis, which is a severe form of inflammatory bowel disease secondary to Clostridium difficile.
Now, clostridium difficile also called c diff, or CDI can lead to many deaths. In fact, there’s different statistics depending on what you read here in the US approximately, you know, 29,000 people annually, 500,000 infections. I’ve seen papers that discuss a little bit lower than that. But either way, there’s way too many people that die from clostridium difficile Infections and way too many people get the infection that can just cause health issues.
And so one of the things that can lead to clostridium difficile infections is antibiotic use that tends to disrupt the microbiome. And then you get the secondary expression of the clostridia. As I mentioned, pseudo ous colitis, toxic mega colon, and then clostridium difficile induced diarrhea are, you know, fairly common.
Now, the primary agents of toxicity of clostridium difficile in the digestive system are what are called toxins, A and B. And the discovery of these toxins in relationship to pseudo ous colitis goes way back to the late seventies. They know also that pseudo membranous colitis is a frequently acquired problem in the hospitalized patients who get c difficile exposure through spore contamination that might come from other patients or even healthcare workers. And so all groups of antibiotics can be linked. Usually things like cephalosporin, penicillium, clindamycin, for example, are more commonly associated with C difficile infections.
So what’s happening is, is the clostridium difficile gets into the digestive system, it’s moving through the small intestine, and then towards the end of the small intestine in the ileum, it encounters bile. And bile is a triggering mechanism for the spore of Clostridium to basically break down. Calcium can also be a trigger as well. And so as the organism is moving out of its spore form into what’s called a germination outgrowth phase, it’s now releasing its internal toxins like toxin A and B that have a primary toxic effect in the large bowel, the colon.
Now the unique thing about clostridioides difficile and other clostridia bacteria is it can reform a spore, so what’s called a SPO agenesis effect. And then it’s moved out of the body, it the stool. Now stool testing has still exists as a primary way of assessing for Clostridium difficile toxin A and B. So we can see a couple different lab examples here from different stool tests looking at the detection of toxin A and B, again, as the primary virulent toxicity factors within the gut.
Virtually all of the research on c difficile is focused on the intestinal damaging strains. Toxin negative strains of C difficile are considered non-pathogenic for intestinal disease. And that’s an important point. There are many different strains of clostridia. It’s not just one bacteria. There’s different types of them. Not all cause bowel disease. And so again, most of the research has been done on c difficile in relationship to the types that are causing bowel problems.
But we know that the organic acids test that mosaic offers has different clostridium markers that are reflective of problems in the digestive tract, but these particular compounds are not having necessarily a direct effect on the gut. They’re having an adverse effect more in the nervous system. So that would be 4-Hydroxyphenol, acetic, H-P-H-B-A. But understand that not all c difficile are causing bowel disease.
So let’s turn our focus real quickly to the organic acids test. So the organic acid profile is looking at different organic acids. These are chemical compounds that get excreted in us as mammals. That is a reflection of our metabolism. They get concentrated in the urine as a reflection of what would be essentially circulating in the blood. Lactic acid, for example, is an organic acid. And so organic acids are compounds that contain carbon and hydrogen always, but they might contain oxygen, they might contain sulfur or phosphorus or nitrogen depending on what type of organic acid they are.
Now, if you look at page one of the organic acid test, there’s three sections, yeast, fungal, bacterial, and Clostridium. And so it’s important to keep in mind that Clostridium is not a standalone problem for most people. It’s existing within the digestive system in individuals who often have other bacterial imbalances, microbiome diversity issues, or even fungal problems. And that’s one of the nice things about doing the organic acid test, is it helps to detect some of these other imbalances in the digestive tract. What you want to pay attention to though is particularly the H-P-H-P-A, but any of those Clostridium markers is significant.
We’re gonna focus a lot though on H-P-H-P-A.
So I actually took these slides from the OAT lecture I do for the Mosaic Edge organic acid test seminar. So this actually came from a teenage boy who had attention deficit problems. He had some mold exposure, and you’ll notice that, you know, the yeast and vagal markers, which is linked to candida. Aspergillus, were both elevated, but he also had two of the four Clostridium markers high, the H-P-H-P-A.
Now remember, these are neurological toxins mostly. It doesn’t mean that he couldn’t have some digestive system problems too, but we’re gonna look at these things in relationship to how they affect the nervous system. The most common one is H-P-H-P-A. It shows up at about, you know, 80% of the time when one of these Clostridium markers is high. For Creole is less common. Notice that for Creole does get produced by C. difficile. But again, there’s many different types or strains of C. difficile.
So the issue with these particular toxins, like for Creole for example, is that they can interfere with tyrosine metabolism. So this was actually from the Journal of Medical Microbiology in 2008, and it says here, C. difficile is a bacteria that is able to ferment P Creole. So P Creole is another name for four Creole, which is a phenolic compound that’s toxic to other microbes. So this particular compound gets produced as a competitive compound against other competing Clostridium bacteria.
One of the problems with Creole is that it is an inhibitor of the dopamine beta hydroxylase enzyme. Now, dopamine beta hydroxylase is what converts dopamine to norepinephrine within the nervous system. This is not just in the brain, this is in the nervous system in general throughout the body. And so what happens is, is the Creole binds to the enzyme and renders it inactive. So we get a decreased conversion of dopamine to norepinephrine.
Now, there are other compounds that can have a similar effect or same effect. Actually, H-P-H-P-A is also an inhibitor of dopamine beta hydroxylase. Here’s our cresol that comes from Clostridium difficile. It takes tyrosine and converts it into Creole. That’s what the organisms are doing. So whether we’ve got Creole or H-P-H-P-A, we know that there can be an adverse effect on dopamine beta hydroxylase. And that’s the enzyme that converts dopamine to norepinephrine.
Norepinephrine is important for energy production, for example, for maintenance of good cardiovascular function. So if nothing else, just remember that the presence of these particular organic acid compounds that we can measure off the organic acid test can inhibit the dopamine beta hydroxylase.
Now, H-P-H-P-A is important in this discussion because there’s other things that we’re gonna talk about with regards to H-P-H-P-A. If you are a practitioner and want to get into this information at a deeper level, I would strongly encourage that you participate in one of the one day seminars on organic acid test fundamentals that I teach through Mosaic Edge.
So the next one scheduled is actually Friday, March 1st. And so this is an all-day seminar that goes through the different aspects of the organic acid test. Some of it we discuss issues with regards to clostridia. So for more information, go to mosaicdxedge.com.
Now, turning our attention back to this individual I’ve mentioned before, who has attention deficit problems. This is a teenage kid. When we look at the bottom of page three of the organic acid test from Mosaic, there is the neurotransmitter section. I mentioned previously that the clostridia markers can inhibit the dopamine beta hydroxylase. And when that happens, you’ll often see an increase of the dopamine metabolite chemical called homovanillic acid.
So you’ll notice that this is elevated in this individual. So what’s happening is that enzyme, that DBH dopamine beta hydroxylase enzyme, is being interfered with. Now, there are some problems that occur when dopamine is elevated over a prolonged period of time, which I’ll discuss a little bit later.
One of the other things that we have to pay attention to in this particular discussion is the presence of clostridia and its potential to interfere with mitochondrial function. On page three of the organic acid test, there’s a number of sections that are linked to mitochondrial activity. And you’ll see in this individual, he’s got quite a few markers that were elevated indicating Kreb cycle and overall mitochondrial dysfunction.
One of the things that clostridia can produce is something called propionic acid. And propionic acid interferes with the Kreb cycle. So this is actually the Kreb cycle inside our mitochondria, and essentially it shuts down the first half of Kreb cycle activity.
Why is that a big problem? Well, it’s the Kreb cycle that segues over to another system in our mitochondria that produces ATP that gets compromised.
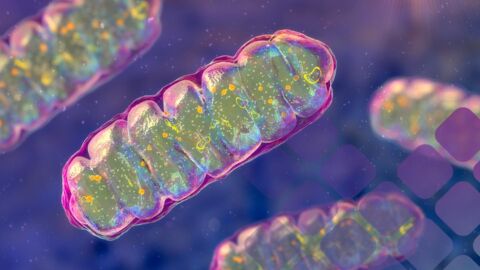
So I wanna turn our attention real quickly, just as a brief overview of the powerhouse of the cell, and that would be the mitochondria. So the mitochondria are known as the energy production factories that produce large amounts of adenosine triphosphate, ATP. So that is our cellular energy currency that our cells of our body use.
Now we need a massive amount of ATP on any given day just for normal function of our brain, nervous system, our heart, our digestive system, our musculoskeletal system, et cetera. And when problems occur in the mitochondria, that can happen either because of dysregulation intrinsically with regards to biochemical sequencing, environmental toxins, nutrient deficiencies, genetic factors, et cetera—our health can be compromised.
And so mitochondrial dysfunction gets triggered by many different types of things. Ultimately, we get a decrease in the production of this ATP chemical, which again is the energy currency.
One of the main things that leads to a depletion of ATP production is anything that disrupts the normal function of what’s called the inner mitochondrial membrane. Because embedded in the inner mitochondrial membrane is something called the electron transport chain. And reduced flow of electrons through that electron transport chain will decrease the ability for the mitochondria to make ATP.
And this causes problems in a wide variety of different disorders and diseases—from neurodegenerative diseases like Parkinson’s, Alzheimer’s, Huntington’s, ALS, to cardiovascular problems, to metabolic issues, autoimmune, even autism, psychiatric conditions, gastrointestinal problems, cancer, you name it. Really, there isn’t any type of chronic health issue that exists within us that doesn’t have some connection to mitochondrial problems.
And the mitochondria are very adept at taking foodstuff substrate that we eat, whether it’s proteins, carbs, or fats, and converting it into energy. Now we get a lot of ATP production when we metabolize fat. We get a decent amount as well by the conversion and use of carbohydrates and proteins.
We’ll talk about acetyl coenzyme A here shortly, because this is an important chemical as a segue for certain proteins, fats, and carbohydrates to make their way into the mitochondria for ATP production.
From a very basic standpoint, glucose gives us a decent amount of ATP. So essentially we get anywhere between 36 to 38 ATP produced per molecule of glucose. And so whenever we come in contact or consume glucose, for example, glucose gets converted to pyruvate and pyruvate gets converted into acetyl coenzyme A that enters the Kreb cycle, that enters the electron transport chain.
Now, about 5% of our ATP production just comes from glucose to pyruvate conversion. We get an additional 5% through sequencing through the Kreb cycle, but we get the major bulk of our ATP produced within the electron transport chain.
Now, when we look at the mitochondria—so this is a mitochondria here—it’s got different things happening going on here, different layers, different membranes. So it has an outer membrane and an inner membrane. The outer membrane has its own function. The inner membrane has its own function as well.
And one of the things is that the membranes create a particular space called the intermembrane space. And that intermembrane space is where hydrogen ions, also called protons, accumulate. They get pumped out of the matrix into this inner membrane space, and they essentially accumulate over top of this particular large complex called ATP synthase. And the influx of the protons back into the matrix is what creates or induces the formation of ATP.
Now, the Kreb cycle is connected to the electron transport chain by a couple different chemicals. The electron transport chain is this complex that is embedded inside or internal within the mitochondria in the inner mitochondrial membrane. So the electron transport chain is situated inside the inner mitochondrial membrane.
And so anything that disrupts—okay, here’s the inner mitochondrial membrane—anything that could disrupt the integrity of the inner mitochondrial membrane will disrupt the overall function of the electron transport chain.
And the easiest way to think of the electron transport chain and what it does is that it’s transporting electrons through a chain reaction. So it’s moving electrons down this particular—these complexes—with the end goal to take oxygen and convert it to water at the same time out-pumping protons into the inner membrane space.
And so these protons, these hydrogen ions, accumulate over top of this last complex called ATP synthase. And as these protons move back into the matrix, it brings together the formation of ATP. And this is happening every second of our lives.
And one of the things that’s important to understand is that cells that are highly metabolically active—so our brain, our nervous system, our heart, our cardiovascular system, our musculoskeletal system—each cell contains thousands of mitochondria. Each mitochondrion contains multiple thousands of these different electron transport chain complexes. And so we’re producing massive amounts of ATP per cell throughout our entire body, every single moment of our lives.
And when we have compromised mitochondrial function that’s affecting one or more of these systems, we can have different types of problems that come about.
Now, one other interesting aspect of mitochondria is this particular chemical called cytochrome C, which I highlighted here in red. Cytochrome C sits between complex III and complex IV, and it shuttles electrons over to complex IV for their final contribution to reduce molecular oxygen to water.
When we get instability of the inner mitochondrial membrane, and that instability is dramatic enough, the cytochrome C will come off of the inner mitochondrial membrane. It will leak out of the mitochondria, and the cell of our body where that’s happening recognizes that as a problem.
And so when we get enough leakage of cytochrome C moving into the internal aspects of the cell, it interacts and triggers a cascade of reactions of different enzymes that trigger something called apoptosis. Apoptosis is a cell suicide signal. Essentially, this is a signal to say, okay, we’re done. This cell needs to eradicate itself from the population.
Now, there’s many things that can cause disruption of the inner mitochondrial membrane: nutrient deficiencies, inflammation, oxidative stress, toxins. Those toxins could be chemicals, heavy metals, mold, mycotoxins—a wide variety of things.
And so depending on where the mitochondria are being affected in the body—if it’s in the brain, we’re gonna manifest with brain problems. If it’s in the heart, we’re gonna manifest with cardiac issues. If it’s in the liver, we can develop liver problems. If it’s in the digestive system, we can obviously develop digestive problems. And so gastrointestinal disorders often can be linked to mitochondrial problems within the digestive system.
And of course, there are genetic diseases that create problems as well. But just keep it in mind that mitochondria don’t necessarily need to be affected all over the body. They can be affected in regional areas that are causing problems or that manifest as problems.
Now bringing it back to the discussion of clostridia: propionic acid, as I mentioned before, is linked to clostridia bacteria. And propionic acid is known to interfere with different steps within the Kreb cycle that exists within our mitochondria. And so propionic acid has been seen in mitochondrial dysfunction linked to neurodevelopmental conditions like autism.
And this is an important understanding because propionic acid is actually linked to H-P-H-P-A, which we pick up on the organic acid test.
So let’s shift our gears now to autism.
And as a general overview, we know that autism, in order to be classified essentially or diagnosed with autism, we’re looking for six or more identifiers from the three major categories of social interaction problems, communication, and repetitive and stereotypical behavior issues. So a child essentially who gets the diagnosis will have problems in all three of these different categories.
Now, one of the other things that’s important to understand about autism is that they are often affected by different comorbid conditions. And this is an old slide that I used from many of my lectures in the past. Even the Centers for Disease Control recognizes the high prevalence of comorbid conditions—from ear and respiratory infections to a tendency more for allergies and other allergic reactions, to sleep problems, to headaches, to seizures, and even gastrointestinal disorders.
And honestly, this is just a partial list. But the point is, these comorbid conditions are often caused by underlying biological problems and can contribute to worsening autistic states—and in some cases, could even be a potential cause in some individuals.
So there’s not just one cause, for example. It’s a multifactorial problem, but the gastrointestinal system plays a big role. If nothing else, gastrointestinal problems are often a major exacerbating factor in an individual’s autistic condition, particularly with regards to behavioral issues.
And so this was actually from a paper in 2012 in Pediatrics:
“If the gastrointestinal disorder is recognized and medical treatment is effective, the problem behaviors may diminish. When abdominal pain or discomfort is a setting event, psychotropic medications are likely to be ineffective.”
So the point is not to just throw meds at these kids; it’s to understand that maybe their behaviors could in part be occurring because of underlying digestive system problems.
And there’s many different types of digestive issues that can exist in autism, from gastritis to reflux to colitis to irritable bowel. Constipation is a major problem. Constipation can come about because of clostridia bacteria. So can motility problems. Many of these kids have a lot of food sensitivity and allergies—even SIBO (small intestinal bacterial overgrowth) is something that is seen in this population of patients.
Now, one of the things that Dr. Shaw, who originally started Great Plains Laboratory, recognized is that many autistic individuals had very high levels of a particular chemical called H-P-H-P-A. H-P-H-P-A stands for 3-hydroxy-3-phenylpropionic acid. And in the autistic kids that he’s tested and has been seen over the years, autistic individuals often have much higher levels of H-P-H-P-A than neurotypical kids of the same or similar age. They also seem to be very sensitive to the presence of this particular compound.
Now, this is not just a unique issue in autism. This was actually a paper that was looking at very high levels of this clostridia compound in a young woman with acute schizophrenia and psychosis. In fact, her levels were massive—almost 7,500. And I’ve actually personally never seen a level that high. So that’s a really, really large amount of this particular compound.
So I want to turn our attention to a new article that came out just this past year from Dr. Bill Shaw—PhD William Shaw—who was originally the founder of Great Plains Laboratory. And this was an article in Integrative Medicine, May 2023, and you can actually get a copy of it online for free at the domain address you see there on your screen.
So it’s called:
Inhibition of the Beta Oxidation Pathway of Fatty Acids and Dopamine Beta-Hydroxylase by Phenol Derivatives of Short Chain Fatty Acids from Gastrointestinal Clostridia Bacteria as a Major Cause of Autism.
So, not a short title—but I would strongly recommend having a copy of this article.
Now, Dr. Shaw has also done lectures through Mosaic Edge, and he has a couple lectures that are also available through New Beginnings Nutritionals’ webinar libraries. So you can go to New Beginnings Nutritionals—nbnus.com—if you want to get into his specific information on the information I’m going to share as an overview through these two particular webinars.
This begins with fatty acid metabolism. So I’m not going to go into all the different aspects of fatty acid metabolism—that in itself is an entire lecture. But what’s important to understand is there’s different ways the cell attacks a fatty acid for metabolism: something called beta oxidation, omega oxidation, etc.
Remember, fatty acids—like carbohydrates and certain proteins—can enter the metabolic pathway for energy production. But in order to get there, they have to be converted into different compounds that can be sequenced into the mitochondria for particular purposes and for ease of use.
So as an overview again, fatty acids can enter different pathways to become something called acetyl coenzyme A. So can carbohydrates, and so can certain proteins. So acetyl coenzyme A is a major entry point into the Kreb cycle. The Kreb cycle is also called the citric acid cycle.
Once the substrate is spun through the citric acid cycle, it enters the electron transport chain for ultimate production of ATP. If you are familiar looking at an organic acid test, you’ll know that under the ketone and fatty acid oxidation section, many of these markers are often elevated in individuals with autism. They can be elevated in other individuals too.
Now, the chemistry behind these is complex, and so we’re not going to get into all of that. But what’s just important to understand is that when many of these markers are elevated, it is indicating that the cells of our body are having a difficult time properly processing fats for energy production.
These first two markers here are what are called ketogenic acids. So sometimes these actually just become elevated by consuming a high-fat diet or even a ketogenic diet. There’s some other reasons they can be high that I’m not going to go into in this lecture.
The markers below—4-hydroxybutyric, ethylmalonic, adipic, suberic, etc.—have their own unique pathways. The bottom line is that for most people, when these markers are elevated, it’s often worthwhile to just administer or take (if yourself) some L-carnitine. And L-carnitine is a specific type of nutrient that assists the cell in the transport of certain length-chain fatty acids for proper internalization and metabolism of fats.
Now, that doesn’t always account for certain genetic disorders, for example—there might be problems—but by and large, for most people, carnitine can sometimes be a beneficial nutrient. And so that always needs to be correlated with your own particular health concerns, for example. But that is sort of a general rule.
Now, what’s interesting in the context of this discussion is coenzyme A is dependent on vitamin B5. So the production of coenzyme A, which is our precursor to acetyl coenzyme A, means it needs to get converted by B5 metabolism—also called pantothenic acid.
Now, as you can see, there’s a lot of enzymes that are in play that help convert pantothenic acid into coenzyme A, and there are certain genetic conditions where some of these enzymes are adversely affected.
A particular form of pantothenic acid called pantethine—which is essentially right here—tends to bypass some of the more common genetic variants that might affect the conversion of pantothenic acid to coenzyme A.
In fact, I just recently had discovered in an autistic individual that they have a mutation in this particular enzyme, P-P-C-D-C, which is the phosphopantothenoylcysteine decarboxylase enzyme. And that particular genetic defect can affect the production of coenzyme A.
Well, why do we need coenzyme A? One of the reasons is to produce acetyl coenzyme A that helps to move food substrate into the mitochondria.
So in this particular individual, what we did is we bypassed the defect and just gave pantethine instead of pantothenic acid. There’s no set amount that I know of for each particular circumstance—everybody is sort of unique—but generally, about 500 milligrams per day I think is a reasonable amount to consider.
By the way, this was the first time that I had seen this particular genetic variant, and that I think was certainly important to understand a little bit more about what can happen downstream from pantothenic acid if we can’t get proper conversion into coenzyme A.
So coenzyme A is necessary in what’s called a group carrier—an acetyl group carrier—to help form acetyl coenzyme A and other related compounds. If you remember nothing else, this chemical is important for energy metabolism within the mitochondria, and it’s linked to many different types of pathways that affect Kreb cycle activity and mitochondrial activity as well.
It also turns out that coenzyme A is important for the production of fatty acids, certain fatty acids, metabolism of cholesterol, and even acetylcholine, interestingly enough.
So what does this have to do with the organic acid test?
Let’s come back now to the Mosaic organic acid test and look specifically at H-P-H-P-A, the most common Clostridium marker on the OATs that gets detected. Here’s the structure of 3-hydroxy-3-phenylpropionic acid. So its base structure contains a six-carbon hydrocarbon ring—a benzene ring—and when we attach a hydroxyl group to it, it becomes a phenol. So this is called a phenyl group, and then propionic acid is attached to carbon one.
It turns out that Clostridia bacteria—certain ones—produce this as its main chemical influence or metabolite, if you will, in the digestive system. And we can pick this up on the organic acid test. And if we understand what it does already, we know that it can inhibit dopamine beta-hydroxylase. We also know that propionic acid in autistic individuals can also bind to some of the Kreb cycle metabolites themselves.
So we’ve got a bunch of things going on here.
We can get inhibition of dopamine beta-hydroxylase. We can also get direct interference with the Kreb cycle. So in this particular article, what Dr. Shaw is discussing is there is a potential, with regards to the existence of H-P-H-P-A and the existence of Clostridium bacteria producing these compounds, to sequester or reduce the available free coenzyme A that gets produced through pantothenic acid metabolism or B5.
Now, I’m not going to go through all the chemistry—it is complex, for sure. So the main point is to understand that when you see H-P-H-P-A, it doesn’t automatically mean in every single case that we’re getting severe dopamine beta-hydroxylase inhibition, or that we’re getting severe mitochondrial problems because of the propionic acid, or that we’re getting mass reduction of acetyl coenzyme A—but the possibility and potential exists.
And so as practitioners, we need to understand that the presence of H-P-H-P-A isn’t really having a benefit. It has the potential of causing problems. And the longer it hangs around, the more potential problems—or problems—it can create.
So it is beneficial to try to get rid of it as best as possible because it’s not going to cause benefit—really, only downstream has problems.
There are a couple of points as we come toward the near end of this discussion. One is that these Clostridia compounds, H-P-H-P-A and 4-creosol, are the two most common ones you will see on the organic acid test. They are direct inhibitors of dopamine beta-hydroxylase.
And as a side note, there are other Clostridia compounds and other phenol or phenolic-type compounds that likely also inhibit that enzyme. So that’s for another discussion.
4-creosol is important, but in this particular discussion, the creosol doesn’t appear to be a sequesterer of free coenzyme A—that is reserved for H-P-H-P-A.
So it’s not to make it sound like 4-creosol is benign—it’s not. It has its own issues. But it’s the H-P-H-P-A that’s really relevant in this particular discussion with regard to coenzyme A.
So what’s happening?
We get a decrease in what’s called beta oxidation. And that is a very important sequence of fatty acid metabolism. The cell then becomes reliant on something called omega oxidation. Now, that’s sort of an alternative pathway through these sequencing events. If we don’t initiate fatty acid metabolism through beta oxidation, we don’t get maximal fatty acid metabolism conversion—and that can ultimately affect energy production through the mitochondria.
Now, we already mentioned that coenzyme A is important for acetyl coenzyme A production, which helps in moving carbohydrates, fats, and certain proteins into the Kreb cycle. Well, it turns out that coenzyme A is also important for cholesterol production.
So if our coenzyme A is being bound up, we’re going to run a risk of having low cholesterol. So we’re going to start there, and then I’m going to come back to this particular slide and hit on a couple of other points.
Alright, so it’s the sequestration of free coenzyme A that is a concern in this part of the discussion.
So I took this particular slide from my advanced OAT mastery course. This was specifically looking at leucine metabolism. We’re not going to pay attention to that. I just want you to pay attention to HMG coenzyme A.
So notice there’s a coenzyme A— in fact, there’s a bunch of coenzyme A’s throughout this entire sequence of events. Well, remember, B5 is needed to make that coenzyme A. But it’s right here—okay? We make cholesterol through what’s called the mevalonate pathway that comes off of this HMG coenzyme A.
So if we don’t have coenzyme A to connect to these chemicals, that can compromise our cholesterol metabolism.
Now, when the lab was still Great Plains, they had done an internal study of a group of autistic children and found that a fair amount had low cholesterol—below 160. And there was a certain subset—about 17–18%—that had extremely low cholesterol, below 100.
The average I’ve seen in my practice with autistic individuals is you probably run 110 to 120 on their cholesterol in milligrams per deciliter. And a lot of the research has shown that looking in the ballpark to be kind of around 160, for example, in milligrams per deciliter with regard to total cholesterol.
So again, fats, carbohydrates, and proteins can get converted into acetyl coenzyme A. Now acetyl coenzyme A is necessary for the production of something called 7-dehydrocholesterol. 7-dehydrocholesterol gets converted into cholesterol through an enzyme called 7-dehydrocholesterol reductase.
There’s a genetic disorder called SLOS—the Smith-Lemli-Opitz syndrome. What I want you to pay attention to isn’t so much the SLOS or the 7-dehydrocholesterol—it’s just cholesterol and the different things it’s connected to.
Cholesterol is needed for bile formation, for fat digestion, for vitamin absorption—particularly fat-soluble vitamin absorption. It’s needed to help produce steroid hormones—many sex and adrenal hormones as well.
In relationship to autism, it’s important because it activates something called Sonic Hedgehog.
So what exactly is Sonic Hedgehog?
Well, I’ll get to that in a second. First, let me briefly wrap up on Smith-Lemli-Opitz Syndrome (SLOS). These kids tend to have extremely low levels of cholesterol. Certain studies have shown that some of them actually have characteristics of autism—they lack speech, can have severe behavioral problems, and show high sensitivity to UV light, for example. Often, they have digit formation problems. A unique characteristic of SLOS kids is a Y-shaped toe between the second and third toes of their feet.
Now, let’s come back to the Shaw article.
We know that a decrease in free coenzyme A can be a problem in autism, and it can occur because of the existence of H-P-H-P-A. A decrease of free coenzyme A can compromise cholesterol production.
The other thing that can happen with a decrease in coenzyme A is we get a decrease of palmitic acid. And that also becomes important because that in itself is also linked to Sonic Hedgehog problems.
So let me first touch on palmitic acid, and then I’ll come back and we’ll finish up talking about the role of Sonic Hedgehog.
Palmitic acid is a 16-carbon saturated fatty acid, and it is named after the most common source, which is palm oil. It’s often elevated in autism, even though an autistic individual’s diet may not be excessively loaded with palmitic acid above the general population.
Now, palmitic acid is found in many different types of oils. It’s very high in palm oil, but it can also be found in beef, milk, butter, soybean oil, and other sources.
As a side note—there are pro-inflammatory aspects of too much palmitic acid. So palmitic acid issues can also become a problem in metabolic syndrome, diabetes, and cardiovascular illness as well. Again, that’s a whole other discussion.
Now remember, in order to get optimal fatty acid metabolism through beta oxidation—including palmitic acid—we need an adequate amount of coenzyme A. And the coenzyme A becomes essentially compromised because of the existence of H-P-H-P-A.
So we need coenzyme A in order to produce something called palmitoyl coenzyme A, and that would essentially be the proper form of coenzyme A that is needed to activate Sonic Hedgehog.
So what’s happening with regard to H-P-H-P-A is that it’s potentially interfering with fatty acid metabolism itself—occupying the coenzyme A that’s needed by these other metabolic enzyme systems for proper cellular metabolism. That’s in addition to its toxicity issues at the dopamine beta-hydroxylase level.
And we can then also look at some of the other factors and other Clostridia problems that have their own issues within the digestive system. But if we just focus on H-P-H-P-A and expand our view of its potential problems, we now can see that it affects neurological function through DBH inhibition, but it can also affect mitochondrial activity and fatty acid metabolism by sequestering coenzyme A that’s needed for overall metabolism.
So let’s just come back now and take a different look at what this whole discussion brings forth when we look at the relationship of cholesterol, palmitic acid, and Sonic Hedgehog.
Sonic Hedgehog is a signaling molecule that’s important in embryonic development—particularly with regards to the central nervous system, which includes the brain, limbs, and digits. Now, it’s not just something that’s produced in the embryo—it’s produced in all of us throughout our lives. So it plays an ongoing role into adulthood, and it’s important for differentiation, proliferation, and maintenance of organ tissues.
The way I think of it—whether it’s absolutely correct or not—is that in order for our body to maintain normal differentiation and regeneration (or orientation) of our anatomy, we need proteins that get constantly produced and modified to continue to lay down these normal templates of anatomical structure. That includes the nervous system, and it plays a big role in the brain and nervous system.
So Sonic Hedgehog is involved particularly, again, in early development of the embryo with regards to the brain, nervous system, limbs, and digits. But it exists as an ongoing stimulus for maintenance of those tissues.
Abnormal activation or function of Sonic Hedgehog—when there’s some sort of problem—has actually been linked to different types of neurological problems, as well as certain types of cancers: brain cancer, breast cancer, liver, gallbladder, and even certain skin malignancies.
Now, these are severe malformations of Sonic Hedgehog. These are looking at genetic-level problems. One of the things to recognize is that one of the jobs Sonic Hedgehog does is to help with proper orientation of cellular formation within an embryo. And one of those things is within the brain and the orientation of our eyes, as well as proper orientation and formation of digits.
Unfortunately, certain kids who have severe manifestations of Sonic Hedgehog problems from genetic defects can develop a cyclops eye—essentially, sometimes they only have one eye or malformed eyes.
This is just a paper that was looking at Sonic Hedgehog’s involvement in craniofacial and limb morphogenesis. So here we can see Sonic Hedgehog is responsible for laying down a template for normal proliferation of teeth. Here, it’s laying down formation and guiding the proper formation of the front of the face, the head, and the orientation of the eyes.
Here we can see Sonic Hedgehog is involved in laying down the pathways and orientation for proper digit formation—that would be our hands and toes as well. This was a mouse, essentially, where there was a Sonic Hedgehog problem genetically. And we can see poor digit formation. In this particular mouse, we can see no digits were formed. And then in a child, malformed digits.
This was just a mouse study that looked specifically at the cerebellum—but it does have relevance for autism, since that is our topic. Sonic Hedgehog signaling is required for expansion of granule neuron precursors, particularly in the cerebellum.
It says Sonic Hedgehog is produced by Purkinje cells of the cerebellum. Now remember, Sonic Hedgehog is being produced by Purkinje cells, and that’s important because those cells are helping guide normal anatomical formation of brain structures. But there’s another role of Purkinje cells, which is also very interesting.
We know that the cerebellum is often an area in the brain of autistic individuals that is compromised. There are other areas too, but the cerebellum plays a big role. It’s involved in motor skill, proprioceptive orientation, sensory control, and balance. Cerebellum problems can affect attention when shifting from one task to another. It can affect gait. It can affect proprioceptive regulation within the nervous system.
What’s interesting about problems in the cerebellum is that Purkinje cells themselves also produce gamma-aminobutyric acid—or GABA. And GABA inhibits certain neurons that reduce nerve cell impulses.
So one of the other aspects of Clostridia bacteria—by the way, I don’t have the slide here, but I probably should have put it in—is that it’s been shown in studies in autism that certain Clostridia toxins can find their way through the vagus nerve into the brain, specifically the cerebellum, and adversely affect Purkinje cells.
There’s a paper that was co-authored by researchers at Harvard and the physiology department at the University of Warsaw. They were looking specifically at Clostridia toxins being produced in the digestive tract that traverse the gut via the vagus nerve into the brain and adversely affect Purkinje cells with a decrease in the production of GABA.
In that particular paper, they were looking specifically at autistic individuals with high levels of anxiety and panic. Well, GABA is an inhibitory amino acid and neurotransmitter of the brain. So it’s going to essentially have a regulatory effect on nerve impulse transmission.
When we get a dysfunction in Purkinje cells, we can now look at it as more than just a GABA situation. We can understand that a problem at the Purkinje cell level—which could be induced, in part, by Clostridia—can cause a reduction in GABA. But we can also see where problems in the Purkinje cells in the cerebellum could also decrease their production of Sonic Hedgehog.
So what Dr. Shaw described is also the fact that Sonic Hedgehog is incredibly important for normal production throughout our lives, as a way of maintaining normal tissue structure and orientation—particularly in the brain and nervous system.
Sonic Hedgehog exists in what’s called a pre-pro form. It has an N-terminal amino group (NH₂) and a carboxy-terminal side (COOH) with a carboxylic acid. These sides flank a sequence of amino acids. This pre-pro form gets broken down into a specific section—amino acids 24 through 179—and this becomes the active form of the Sonic Hedgehog protein.
We need palmitoyl coenzyme A—derived from palmitic acid—and we also need cholesterol in order to activate Sonic Hedgehog. The palmitic acid gets attached to the amino end (N-terminus), and the cholesterol gets attached to the carboxy end (C-terminus). These two chemical modifications activate the Sonic Hedgehog protein.
This is a common concept in biochemistry—where a molecule is synthesized in an inactive form and then activated by some modification. In this case, Sonic Hedgehog becomes functional when both cholesterol and palmitic acid are attached. These modifications are essential for the molecule to properly signal within the body.
We now know that coenzyme A depletion can negatively affect both of those components—palmitoylation and cholesterol synthesis. So this is one of the downstream effects of H-P-H-P-A production by Clostridia: a potential disruption of Sonic Hedgehog signaling.
Now, I’ve been talking about autism, but please understand that Sonic Hedgehog—as I mentioned before—is produced in adulthood as well. So problems in Sonic Hedgehog signaling have also been seen in other types of conditions, particularly neurodegenerative diseases like Parkinson’s disease, Alzheimer’s disease, etc.
You’ll see a fair number of people with neurological problems who also have Clostridium issues—particularly high levels of H-P-H-P-A. So the organic acid test is not just for autism. It’s critically important for individuals with autism, but it’s also incredibly relevant for patients with other types of chronic health issues.
In fact, I’ll make the case that anybody dealing with some type of chronic health problem should have an organic acid test done—for many reasons: to look at all the different sections on the OAT test, but also specifically to look at these Clostridium markers.
I understand this is challenging information. There’s a lot of complex chemistry here and many interconnected pathways. But as we dig deeper into the usefulness of the organic acid test, and into the toxicity issues related to Clostridia, we can start to see that these compounds have far-reaching effects—especially for patients with complex conditions like autism.
So in conclusion:
The key point is that the organic acid test should be done on anyone with an autism diagnosis, those suspected to have autism, individuals with special needs, or even those without a confirmed diagnosis but who display characteristics. It’s also useful for many others.
If H-P-H-P-A is present, it’s imperative to treat it—whether that’s with botanicals, antibiotics, or other methods—for its eradication. 4-creosol is important as well, but it doesn’t have the same direct relevance in this particular discussion on coenzyme A sequestration.
There are many other foundational nutrients that can support the mitochondria. Various B vitamins—like B1, B2, and B3—are helpful. One of the things I’ve started doing in my practice is incorporating more of the activated form of B5, pantethine, especially when H-P-H-P-A is elevated.
Support for fatty acid metabolism is also important. As I mentioned before, L-carnitine is a nutrient that can help transport fatty acids into the mitochondria.
Antioxidant support may also be warranted—again, not necessarily for directly treating Clostridia, but to reduce any potential oxidative stress at the mitochondrial level.
Microbiome diversification is another critical component. That includes probiotics such as Bifidobacteria, Lactobacillus, and Bacillus species.
It’s important to remember that Clostridium infections are not always a standalone issue in the gut. Often, there are other coexisting problems—parasites, fungal overgrowth, mold colonization, or chemical exposures—that can compromise an individual’s health, mucosal immune function, or microbiome, and reduce their ability to clear Clostridia.
Each of these topics could be its own lecture—on supplements, interventions, treatment protocols—but the purpose of today’s webinar was to go over this foundational material and dig into some of the newer information regarding Clostridia, specifically H-P-H-P-A, its effect on free coenzyme A sequestration, and the downstream impacts on fatty acid metabolism, mitochondrial activity, and Sonic Hedgehog signaling.
What I’ve decided to do, in relation to this talk—and I’ve had this Substack up for a while—is to continue building on this topic through articles and video presentations on my personal Substack. So if you’re not familiar with Substack, it’s a platform for writing and content sharing.
You can find me at drwoeller.substack.com.
I post articles and videos a few times a week. I’ll be diving deeper into this topic of Clostridia, Sonic Hedgehog, fatty acid metabolism, and more.
Also, I have a new course launching in February 2024 called the Clostridia Mastery Course. It’s open to anyone interested in this information. You can visit clostridiamasterycourse.com for more info. This will be an in-depth look at Clostridia—from the content we covered here today to many other related clinical and biochemical topics.
If you’re interested in additional material or our other offerings through Integrative Medicine Academy, you can email us at integrativemedicineacademy@gmail.com or visit integrativemedicineacademy.com for a full list of courses.
Lastly, I’m available for private consultations through my practice. Our website is mysunrisecenter.com, and our email and phone number are listed there as well.
So, I want to thank Mosaic Edge and Mosaic Diagnostics for continuing to sponsor these monthly webinars. I always enjoy putting these together. I know the information can be complex, but the more we hear and engage with these ideas, the more familiar we become with the concepts—and the better able we are to help our patients.
Until next time, I’m Dr. Kurt Woeller.
Thank you so much.