A mold by definition is “a fungus that grows in the form of multicellular filaments called hyphae” (1). One of the most common mold fungal species is aspergillus. In contrast, “fungi that can adopt a single-celled growth habit are called yeasts” (2), which includes the many species of candida. Both candida and aspergillus are types of fungus, but candida is not a mold, and aspergillus is not a yeast. Molds (and other fungus) can produce different chemical compounds known as mycotoxins which are secondary metabolites (3) that can cause disease and death in humans and animals (4). An example of a group of dangerous mycotoxins of aspergillus mold is aflatoxins. These substances are some of the most carcinogenic compounds known in the field of biological toxins (5). Other mycotoxins from various molds such as penicillium, fusarium, and Stachybotrys chartarum are categorized as immunotoxic, hepatotoxic, nephrotoxic, neurotoxic (6). Molds are ubiquitous in the environment and mold spores can inhabit soil, certain food products such as grains, as well as dust particles. Several species of aspergillus, including A. fumigatus and A. niger can grow in damp, humid, and warm environments (7) and may even be found in bedding and pillows (8).
A person’s reaction to mold can range from typical allergic symptoms such as nasal congestion, itching, sneezing, and a mild cough to more severe manifestations linked to mycotoxin poisoning and associated adverse health effects such as immune suppression or organ damage. Listed here is a brief overview of different, but common physical reactions to various components of mold exposure:
Mold Allergy
A mold allergy is an abnormal immune reaction mediated through immunoglobulin E (IgE) production in response to exposure to mold spores or cellular components of the mold. This immune reaction causes various inflammatory chemicals to be produced which can appear as simple nasal congestion, watery eyes, and mild cough, to more severe reactive airway disease and asthma (9).
Mold Infection and Fungemia
When mold spores are inhaled intact, they can embed in lung tissue and cause an infection. This is particularly serious for any individual with immune disorders or other diseases such as asthma, cancer, chronic obstructive pulmonary disease, emphysema, diabetes, etc.
The infection linked to invasive fungus is called fungemia which is defined as a fungus found in the bloodstream. The most common form of fungemia is candidemia linked to invasive candida but can occur from aspergillus invasion. An aspergillus infection is termed aspergillosis and can ultimately lead to invasive aspergillosis (10). A common form of aspergillus is A. fumigatus which is significantly opportunistic in immunocompromised individuals (11).
Mold Induced Hypersensitivity
The most common form of mold hypersensitivity is linked to the direct exposure to inhaled mold spores. It does not matter if the mold spore is alive or dead because reactivity can also occur to hyphal fragments that trigger inflammation in the upper airways, lungs, and systemically. Mold hypersensitivity has been linked to sick building syndrome (12) where people experience heightened symptoms and health problems when they encounter environments known to have mold contamination.
Many research papers have been written about sick building syndrome, including a 2018 review. This comprehensive analysis reviewing 16 previous studies concluded that individuals exposed to molds and associated mycotoxins had “symptoms affecting multiple organs, including the lungs, musculoskeletal system, as well as the central and peripheral nervous systems” (13). The symptoms associated with sick building syndrome could occur in almost anyone with mold illness and is likely associated with mycotoxin exposure and toxicity
Mycotoxins
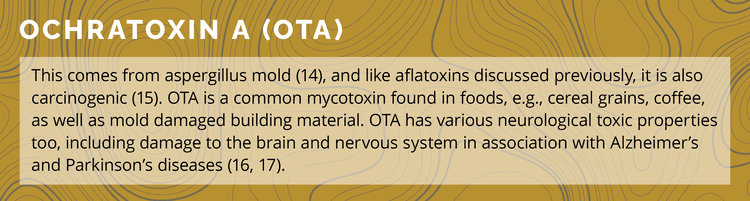
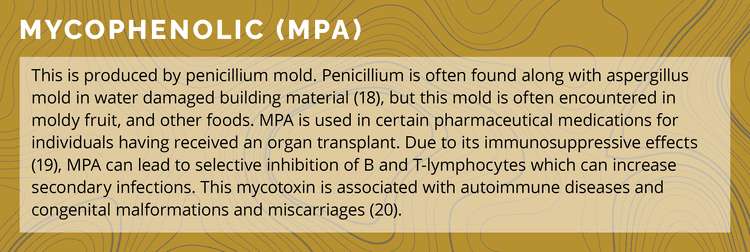
As discussed previously, these toxins of mold as secondary metabolites, have a wide array of negative health effects. There are many different types of medically significant mycotoxins, including ochratoxin A, gliotoxin, mycophenolic, and trichothecenes:
Mycotoxin Testing
There are two popular methods for analyzing the existence of mycotoxins in the body. One is called enzyme-linked immunosorbent assay (ELISA) and the other is liquid chromatography-mass-spectrometry (LC-MS).
ELISA – this method works on a “lock and key” method where a specific antigen (a substance that can stimulate the production of an antibody) is attached to a binding surface such as a polystyrene plate. A matching antibody is applied over the surface of the binding plate which allows the antibody a chance to bind to the antigen. The binding antibody, which is linked to a specific enzyme, then reacts with an added enzyme substrate. The substrate-enzyme reaction produces a chemical change signal indicating a positive match for the identified mycotoxin.
LC-MS – this method utilized by Mosaic Diagnostics is popular in chemical analysis because each technique is synergistically enhanced. The liquid chromatography separates multiple chemical components, while the mass spectrometry provides structural identity of the individual components with high molecular specificity and chemical detection sensitivity. In essence, LC-MS provides high accuracy of chemical detection of seemingly similar appearing compounds.
Both methods help to identify the existence of various mycotoxins, but with the ability for LC-MS to analyze specific chemical configurations it greatly reduces the false positive detection of similar compounds.
Final Comments
The discussion focused on treatment of mold exposure and mycotoxicosis is about as extensive and complicated as they come in integrative medicine. From a simplistic standpoint, if an individual is having allergic reactions to a mold the easiest thing to do is remove oneself from the environment. Anti-allergy medications may provide some temporary relief, but these do nothing to treat an underlying infection or manage the accumulation of mycotoxins. In most cases when it comes to mold illness, the situation is often more complex than a common mold allergy.
The difficulty with long-standing mold exposure is it often leads to systemic toxicities that greatly affect health. Each person needs to be analyzed individually to determine if they are suffering from common mold hypersensitivity, fungemia and/or mycotoxin toxicity.
Because mold organisms can colonize various areas within the human body, e.g., sinuses, lungs, gastrointestinal tract, comprehensive diagnostic approaches often need to be taken to determine at what level someone is affected. This can include performing a Mold IgE Allergy Test from Mosaic Diagnostics which identifies a multitude of environmental molds known to activate IgE antibody production.
The mycotoxin profile, (MycoTOX Profile) from Mosaic Diagnostics evaluates for various medically significant mycotoxins as discussed previously. However, these mycotoxins can exist for long periods of time in the human body even though an individual is no longer acutely exposed to mold. For example, it is possible to have a normal Mold IgE Allergy Test but have elevated levels of mycotoxins.
The Organic Acids Test (OAT) from Mosaic Diagnostics has specific markers found in the Yeast and Fungal section on page one. The aspergillus and fusarium organic acids identify digestive colonization of these mold exposures. When the OAT is done along with a MycoTOX Profile and/or Mold IgE Allergy assessment, these tests may or may not show elevated findings. Therefore, when considering laboratory tests for mold exposure, it is often necessary to do multiple tests, as well as obtaining a thorough clinical history of exposure and symptoms.
It is critical for any practitioner working with a mold-exposed individual to have a broad understanding of the various reactivity mechanisms and adverse health effects of mold and mold toxins.
References
1. Candidiasis. Fungal Diseases. (2019). United States: Centers for Disease Control and Prevention.
2 Moore D, Robson GD, Trinci AP, eds. (2011). 21st Century Guidebook to Fungi (1st ed.). Cambridge University Press.
3. Richard JL (2007). "Some major mycotoxins and their mycotoxicoses – an overview". Int. J. Food Microbiol. 119 (1–2): 3–10.
4. Bennett, J. W.; Klich, M (2003). "Mycotoxins". Clinical Microbiology Reviews. 16 (3): 497–516.
5. Hudler GW (1998). “Magical Mushrooms, Mischievous Molds: The Remarkable Story of the Fungus Kingdom and Its Impact on Human Affairs.” Princeton University Press.
6. Bennet, J.W., Klich, M (2003). “Mycotoxins”. Clinical Microbiology Reviews. 16 (3): 497–516.
7. Latgé JP (April 1999). "Aspergillus fumigatus and aspergillosis". Clinical Microbiology Reviews. 12 (2): 310–50.
8. "Pillows: A Hot Bed Of Fungal Spores". (2017). Science Daily.
9. Fisk WJ, Eliseeva EA, Mendell MJ (2010). "Association of residential dampness and mold with respiratory tract infections and bronchitis: a meta-analysis". Environmental Health. 9: 72.
10. Simicic S, Matos T, “Microbiological diagnosis of invasive aspergillosis.” Zdravnisji vestnik-slovanian medical journal. (2010). Vol. 79, Issue 10, pp. 716–25.
11. McCormick A, Loeffler J, Ebel F (2010). "Aspergillus fumigatus: contours of an opportunistic human pathogen". Cellular Microbiology. 12 (11): 1535–43.
12. Hardin BD, Kelman BJ, Saxon A (2003). "Adverse human health effects associated with molds in the indoor environment". Journal of Occupational and Environmental Medicine. 45 (5): 470–78.
13. Ratnaseelan AM, Tsilioni I, Theoharides TC (2018). "Effects of Mycotoxins on Neuropsychiatric Symptoms and Immune Processes". Clinical Therapeutics. 40 (6): 903–917.
14. Ringot D, Chango A, Schneider YJ, Larondelle Y. Toxicokinetics and toxicodynamics of ochratoxin A, an update. Chemico-biological Interactions, 15 Nov 2005, 159(1):18-46.
15. Annie Pfohl-Leszkowicz, Richard A Manderville. Mol Nutr Food Res. 2007 Jan;51(1):61-99.
16. Belmadani A, et al. (1999). "Selective toxicity of ochratoxin A in primary cultures from different brain regions". Arch Toxicol. 73 (2): 108–114.
17. Sava V, et al. (2006). "Acute neurotoxic effects of the fungal metabolite ochratoxin A". Neurotoxicology. 27 (1): 82–92.
18. Brankica Aleksic, Marjorie Draghi, Sebastien Ritoux, Sylviane Bailly, Marlène Lacroix, Isabelle P Oswald, Jean-Denis Bailly, Enric Robine. “Aerosolization of Mycotoxins after Growth of Toxinogenic Fungi on Wallpaper.” Appl Environ Microbiol. 2017 Aug 1;83(16).
19. Mycophenolate Monograph for Professionals". Drugs.com. Retrieved 28 October 2019.
20. Prossnitz, Eric R.; Barton, Matthias (2014). "Estrogen biology: New insights into GPER function and clinical opportunities". Molecular and Cellular Endocrinology. 389 (1–2): 71–83.
21. Etzel RA (2002). "Mycotoxins". JAMA. 287 (4): 425–7.
22. Kiessling K (1986). "Biochemical mechanism of action of mycotoxins" (PDF). Pure and Applied Chemistry. 58 (2): 327–338.
23. Zorov DB, Juhaszova M, Sollott SJ (July 2014). "Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release". Physiological Reviews. 94 (3): 909–50.