The material contained within this presentation is not intended to replace the services and/or medical advice of a licensed healthcare practitioner, nor is it meant to encourage diagnosis and treatment of disease. It is for educational purposes only. Any application of suggestions set forth in the following portions of this article is at the reader’s discretion and sole risk. Implementation or experimentation with any supplements, herbs, dietary changes, medications, and/or lifestyle changes, etc., is done so at your sole risk and responsibility. Views expressed are those of the presenter and not necessarily those of Mosaic Diagnostics.
Q: Is fungal sinusitis a mold problem?
A: Mold is a type of fungus, so if there is mold in the sinuses then it would be a cause of fungal sinusitis.
Q: Can one beat it with a nasal spray alone as opposed to a whole-body approach?
A: Yes, this is possible if the mold is isolated to the sinuses.
Q: How do we treat it? Apart from remove the toxic mold? Botanicals, antibiotics etc.?
A: Every patient is different. Here’s a good article about diagnosing and treating mold exposure. Here’s a good article about 8 binders for mycotoxins.
Q: If a client has been diagnosed with vasculitis and is not able to pass urine regularly, is this related to a specific nephron structure or general?
A: Vasculitis is inflammation of blood vessels and both arteries and veins can be affected. If a specific blood vessel providing blood flow to a nephron or specific part of the nephron is inflamed this could adversely affect the cells of the nephron and therefore kidney function. Lack of blood flow that is severe can leads to death of cells that could lead to necrosis.
Q: To what extent can renal function recover if the mycotoxins are properly removed?
A: This depends on a lot of factors such as the level of exposure, duration of exposure, underlying tissue damage, healing capacity of the affected cells, etc.
Q: I presume the hepatic function can generally recover more readily.
A: The liver has increased capacity for healing compared to other organs in the body. However, the same or similar factors as mentioned previously with regards to the kidneys applies to the liver or any organ.
Q: I’m assuming that the oxalates Aspergillus can also cause oxalate kidney stones, correct?
A: Yes. If Aspergillus is producing oxalate, and these oxalates find their way into general circulation and into the kidneys they could cause or contribute to kidney stones.
Q: Once you get rid of mold, how long can internal systemic effects last?
A: This depends on a lot of factors such as the level of exposure, duration of exposure, damage that has occurred to tissue function, healing capacity of affected cells, general health of patient, etc.
Q: I think of oxalates as disruptive crystals capable of mechanical disruption of structural components of organelles and membranes. Hence capable of triggering release of those usually sequestered compounds that can trigger apoptosis or necroptosis, etc.
A: I think this is a good description too.
Q: What about when Organic Acids Test mold markers are elevated, but no MycoTOX Profile markers come out elevated?
A: This is a scenario that can happen. Just because Aspergillus appears to be colonizing the digestive system as detected by elevated OAT markers (#2, #4, #5, or #6), it does not automatically mean corresponding Aspergillus mycotoxins will be produced at high levels and detected on the MycoTOX Profile. However, in most cases in my experience (approximately, 80-90% of people) there are corresponding mycotoxins seen.
Webinar Transcript
This is an automated AI transcript of the Webinar video seen above. For the most accurate account of Dr. Woeller’s presentation, please watch the webinar video on this page.
Hi everybody, this is Dr. Woeller checking in here for our monthly sponsored webinar from Great Plains lab. I’m from Integrated Medicine Academy. And I thought what I would do in this particular talk is talk a little bit about how mold and mycotoxins affect certain detoxification organs specifically the liver and the kidneys—so pretty interesting information actually in putting this together.
So if this is the first time hearing me, I have been an integrative and functional medicine physician since the late 90s. I do a lot of education for Great Plains Lab as well as my own online academy called Integrated Medicine Academy.
Spoken throughout the US or as well as internationally, written a number of books. I’m very much involved in education as well as being a practitioner practicing clinician.
Almost a co-founder and education director of Functional Medicine Clinical Rounds, which is actually a membership site for healthcare practitioners who are wanting some assistance on case presentations or case analysis, lab reviews, etc.
And then in my own practice, I’ve worked for decades now with individuals on the autism spectrum as well as other patients with chronic and environmentally induced health issues.
So what we’re going to talk about is the impact, or some examples of the impact—negative impact—of certain mycotoxins on liver function and kidney function. And admittedly, there’s so much information here that we could spend hours talking about the different mechanisms of action that certain mycotoxins have on various organ systems. So some of this will be a bit of an overview, but we’ll get into some specifics too about some interesting aspects as well.
So as a general overview, the kidneys are very important. So primarily the elimination of water soluble products from the blood, some of those actually coming from the liver. And then it’s very much involved in maintaining electrolyte balance as well as maintaining acid-base balance. So when you think about problems that could occur in the kidneys with regards to electrolytes—sodium, potassium, chloride—and acid-base balance, we can start to see that problems in the kidney could lead to other issues in the body that can affect things from a neurologic, cardiovascular standpoint.
Changes in pH—so leading to metabolic acidosis or metabolic alkalosis—are real potentials when we have kidney dysfunction.
The liver is a really large organ, very complex in its physiology. But think of it as the primary organ of detoxification because its role is to take lipid soluble compounds and convert them into water soluble compounds. And there’s other aspects of liver physiology, which we’re not going to get into here, but for the aspect of this particular talk, what we have to think about when we think about mycotoxins is that these are toxins of obviously mold.
That would tend to fall into the grouping of perhaps exotoxins, for example, because they’re not naturally present in our body. But what they do is they can interfere with phase one as well as phase two and even phase three liver detoxification, which I’ll talk about here shortly.
Now interestingly within that intermediate phase is these thiols, and I’ll focus a little bit more on thiols shortly. But we get a lot of thiols by eating garlic or onions or other cruciferous vegetables, for example. And one of the key aspects of just this particular slide, if you look at it, is understanding that there is a wide variety of nutrients—from B vitamins to glutathione to amino acids to phospholipids to antioxidants—that play a role in the various phases.
So I wouldn’t lock into just, you know, thinking that B12 only has an influence in phase one or that glutathione only has a function in phase two. But they do play kind of individual roles in the end result: converting lipid soluble to water soluble compounds so that we can more easily eradicate these toxins through the urine and the stool.
So mycotoxins are of fungal origins. So these are toxins or chemical compounds that have toxic effects that get produced by a wide variety of mold.
And they can create a lot of problems. So very simplistically, they can disrupt cellular processes with regards to protein synthesis. They can damage DNA, they can damage RNA, they can directly affect mitochondria—which I’ll have some examples of—and they can also lead to a depletion of glutathione. But glutathione can also be important in detoxification of some of these mycotoxins.
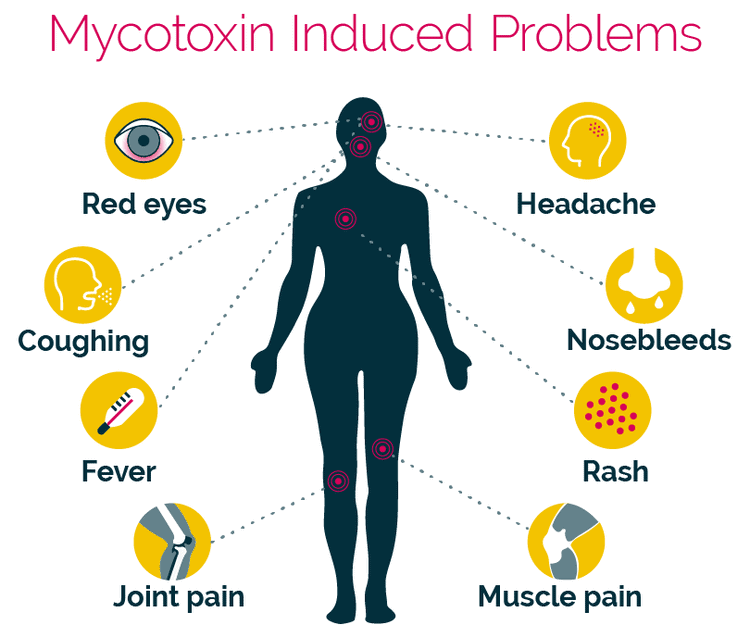
Now this is just a short list of problems that can come about from mycotoxin exposure—headaches to nausea, vomiting, abdominal pain, immune issues, neurological problems, hormone dysregulation, and even cancer. So again, you could create an entire lecture over just that particular topic.
Now some individuals who are exposed to mold may just develop some sensitivity issues. Very common molds that occur indoors—cladosporium, penicillium, alternaria, aspergillus, for example—and it may be that somebody who’s exposed, a lot of us are exposed to aspergillus for example, may just develop some allergic reactivity and that’s it.
In fact, you can actually do an IgE allergy test from Great Plains to actually look at allergy reactions to mold. So that may be what is happening in an individual who has allergic reactions, respiratory problems, sinus issues, for example. And that is fairly common.
Aspergillosis is an infection of aspergillus. So the aspergillus spores can get into the sinuses, they can get into the lungs, and they can cause infection in those particular areas.
Now people who generally are more immune compromised would be more at risk for aspergillosis. And then there are different forms of aspergillosis—things that might reside in the bronchi, things that might reside more in the deeper aspects of the lung, or in some cases the aspergillus becomes invasive. And you have a systemic infection—what’s called invasive aspergillosis.
But all of that, from just an allergic reaction or sometimes mechanical reaction within the respiratory system to the presence of mold spores or an infection reaction from aspergillus, doesn’t necessarily explain the mycotoxin problems.
So in order to pick up on the presence of mycotoxins, you have to do the MycoTOX test. You can’t assume that the mycotoxins are normal if, let’s say, the organic acid test mold markers are normal, or if you do an IgE panel for mold allergy.
So there’s all of these different tests that give us a different viewpoint on the existence of mold or the toxins that mold produces. So in this case, the MycoTOX profile—and you can see in this particular example—we’ve got elevations of a number of different mycotoxins from ochratoxin, gliotoxin, mycophenolic, roridin E, and zearalenone.
Some of these are more common than others. So, for example, the most common mycotoxin to see on this test is ochratoxin. In my experience, probably mycophenolic would be the second most common, maybe gliotoxin coming into close third. You don’t, fortunately, see roridin E or zearalenone, or even the enniatins and beauvericin, for example, all that often, but those particular mycotoxins are problematic, and we’ll talk about a few of them here in the context of this lecture because they can be damaging to the liver and kidneys.
Now remember one thing about the existence of a mycotoxin—and that the presence of a mycotoxin doesn’t automatically mean that your patient is toxic from that toxin—but these mycotoxins are not beneficial. They’re not adding benefit. They have certainly the potential to cause problems, and so usually the longer they hang around, the greater chance that a person is going to develop a negative health outcome from their existence.
But the factors that affect overall health are varied. So age of the individual, the biological sex, can determine some of the susceptibility issues. Other diseases that they may have, certainly other exposures—so there’s compounding problems that can occur when there are other things that a patient is being exposed to, whether it’s chemicals, for example, or metals. You know, there’s information out there too that certain other infections can certainly compound the problem in the presence of mycotoxins.
Candida, for example, would be an example of that. Certainly, poor nutritional status and then just the length of exposure. You could probably add on this too—the amount of exposure would be another determining factor.
So there are some mycotoxins on this particular slide that currently exist on the current form of the MycoTOX profile from Great Plains—so aflatoxin, ochratoxin A, enniatin B, sterigmatocystin, and verrucarin A, for example.
There is in the works an updated or sort of a newer MycoTOX profile that will be coming out. I don’t have the exact date, I don’t want to say, but shortly—I know it’s being worked on—that will have an expanded MycoTOX profile. And so there will be certain mycotoxins on that test that will be very important to detect, that they themselves can have negative influences on liver, kidney, or both.
So, for example, aflatoxins and enniatin B, ochratoxin, and sterigmatocystin—which are on the current version of the MycoTOX profile—can be damaging to the liver. They can also be damaging to the kidneys. Something called H2 toxin and T2 toxin—the relatively similar—are also damaging to the liver and kidneys.
In fact, the thing is this may be sort of an oversimplified slide, in that many of these mycotoxins can be damaging to other organ systems as well. So it’s important to just kind of understand that there’s a broad effect of these mycotoxins that are sort of beyond just what we’re going to discuss here.
So aflatoxins—there’s many different types from B1, B2, G1, G2, for example—and these are toxic compounds that get produced by aspergillus mold. And there’s a number of examples: Aspergillus flavus, Aspergillus parasiticus.
One of the things about aflatoxins is they are damaging certainly to the liver and the kidneys. They can also be carcinogenic, or some of the more toxic compounds found in biological systems.
Enniatin B is a significantly toxic compound of fusarium mold. Fusarium mold is another common mold that contaminates water-damaged buildings, but it can also be found in various foods like grain products.
Enniatin is a damaging mycotoxin to mitochondria, and it also has carcinogenic properties.
I mentioned the T2 and the H2 toxins. These are what are called trichothecenes. I’ll show you a chemical structure of those here shortly. They can be produced by Fusarium as well as Stachybotrys and another mold called Myrothecium.
So trichothecenes are pretty nasty as far as their effects.
Ochratoxins—we see these quite commonly. Again, another toxic compound of Aspergillus. It has carcinogenic properties as well.
Sterigmatocystin is closer related actually to aflatoxin, produced by Aspergillus, but it can also be produced by Stachybotrys as well as Verrucarin A. So in my experience, I don’t see many verrucarins. Don’t see many enniatins and Bs, fortunately, and that primarily goes to the fact that the vast majority of people are not being exposed to Stachybotrys, which is a very dangerous mold and generally from a water-damaged standpoint requires, you know, quite a significant overgrowth scenario.
Although I do have a case of an individual I’m working with who had very profound exposure to Stachybotrys.
So what about some examples of damage that’s happening within the cell, within some of the cellular components that function from a cellular and molecular biology standpoint?
And again, these are examples. These aren’t necessarily all just specific to the liver and kidney—but certainly they would manifest, or can—this is how some of the problems can occur in those organ systems.
So, for example, RNA polymerase. So RNA polymerase synthesizes RNA from DNA. So we have that DNA template and then we create RNA from that through RNA polymerase—or basically what would become messenger RNA.
And that messenger RNA then gets taken out into the cytosolic fluid and then interacts with the ribosome. And that’s where we start to produce proteins. So the protein synthesis component would be occurring within the ribosome.
It turns out that aflatoxins and ochratoxins can also damage DNA. So again, many of these mycotoxins have a damaging effect on RNA and DNA and then also on protein synthesis.
And that’s a big one because many of these mycotoxins like roridin E and verrucarin A are trichothecenes, which get produced by Stachybotrys. And they can have a profound effect—negative effect—on protein synthesis.
Many of these mycotoxins are damaging to the mitochondria in various ways, and I’ll show you a few examples of that. Whenever you think of mitochondrial damage, remember the liver is a high metabolic organ, and so it’s going to have a lot of mitochondria—as well as the kidneys.
But the mitochondria can be damaged in other organ systems as well, including the nervous system, including the immune system, and even the cardiovascular system.
Again, most of these mycotoxins, if not all, will generate some reactive oxygen species at least at some level, and that itself has damaging effects within the cell, within the mitochondria, many times within the nucleus of the cell, again affecting DNA and RNA.
But I want to focus just a little bit on the roridin E and the verrucarin A because these will actually affect ribosomal activity.
So roridin E is considered a trichothecene produced by Stachybotrys. I’ll talk a little bit more about the structure and some of the chemical reactivity of trichothecenes here shortly.
Again, fortunately, we don’t see this marker—at least I don’t—all that often.
Verrucarin A is a very toxic compound. In fact, it’s considered to be one of the more toxic forms of these trichothecene chemicals.
So a trichothecene is this very complex structure. This is called what’s a macrocyclic trichothecene, where it has this additional ring structure out here, and then it’s got this interesting little L-shaped or triangular shaped chemical called an epoxide. I’ll talk about that here shortly.
So the thing to remember about trichothecenes is they’re very reactive chemically. They’re also called amphipathic, so they basically can move in and out of cells quite easily. So they’re transmissible, I guess you would say, between the intracellular and extracellular fluids—which makes them so problematic and so damaging to cell function.
So what is one of the aspects of trichothecene damage of these specific compounds—roridin E and verrucarin? Well, they can damage the ribosome by specifically binding to an enzyme called peptidyl transferase.
And peptidyl transferase is basically involved in helping to transfer amino acids onto an amino acid sequence to form a peptide. So basically, we’ve got our messenger RNA that’s getting read by the ribosome.
And if the sequence of the messenger RNA—which came off the DNA template—is a code that we are now coding different amino acids to make a protein…
So basically, these things are interfering with protein synthesis. So they interfere with either the initiation or the elongation of a peptide chain. Now that has profound effects throughout the cell because the cell functions off of the proteins that are being produced inside that cell, and then other cells are certainly dependent upon that as well.
The mitochondria can be affected. The other thing about some of these trichothecenes is they’ll interact with what are called sulfhydryl groups, which I’ll show an example of here shortly. But that’s important because many amino acids—particularly sulfur-containing amino acids—can become dysfunctional in the presence of mycotoxins.
Oxidative stress—free radicals—pretty obvious that that’s just going to cause widespread damage throughout a cell, whether it’s affecting the cell membrane, the nuclear membrane, the mitochondrial membrane, or the inner workings at various stages or areas within the cell.
So these sulfhydryl groups are very vulnerable to interaction with some of these trichothecene mycotoxins—or all of these trichothecene mycotoxins.
One of the interesting things you can do is just to pull up an image of a cell. And, you know, a graphic image like this doesn’t really convey what’s truly going on inside a cell, because this one only looks like it’s got, what, five mitochondria? And there can be thousands of mitochondria that can exist in a particular cell depending on the metabolic activity of that organ system.
But if we look at a few things, right—so we know that the mitochondria are vulnerable to toxins. We’ve already mentioned how some of these trichothecene mycotoxins can interfere with the ribosome. And so the ribosome is where that peptidyl transferase is active. So dysfunction in the ribosome is going to affect the way a protein is made—so basically it’s going to affect aspects of ribosomal activity that’s sitting upon the rough endoplasmic reticulum, which is where we’re producing protein.
So these little blebs right here along that endoplasmic reticulum—there’s also free-floating ribosomes as well—these can be affected by mycotoxins, which is going to affect protein synthesis.
So the RNA comes out of the nucleus, it goes into the ribosome attached either free-floating or on the rough endoplasmic reticulum. We get protein synthesis. And then the endoplasmic reticulum is important for helping to modify that protein, sometimes folding that protein, and then it gets sent off to the Golgi bodies—or what’s called the Golgi apparatus. And the Golgi apparatus is sort of the final modifications of that protein.
Okay, so you know all of these things need to work in coordination. Now, that protein might just get used inside the cell, or it might be expressed out of the cell.
And I did a lecture a few months back on exosomes, for example, which was pretty interesting in some of the cellular activity with regards to the expression of exosomes and how exosomes are cargoes of a cell that then get transferred throughout the body and have an influence on other aspects of cellular and molecular biology.
If you want to watch that video, you can actually go to Great Plains’ website, go under their webinar library, and then look up the—excuse me here—look up the biological role of exosomes.
I also did a few months back a more expanded lecture on mycotoxin-induced mitochondrial dysfunction inside a toxicity effect. So you can check out—that’s also in the webinar library.
To key off a little bit here on the mitochondria—so the mitochondria play a huge role obviously in the production of ATP.
Trying to find where ATP is—ATP.
And we know that the mitochondria are very sophisticated. There’s a lot of components, but they’re also vulnerable to areas where things can break down. So if we don’t get enough fuel, for example, to feed the mitochondria, that can be a problem. If we don’t have shuttling, transporting mechanisms to get certain things into the mitochondria, that could be a problem.
And ultimately it could lead to a problem in the production of ATP.
The Krebs cycle is very vulnerable to toxicity, as well as our ATP synthase. But the big area I’m going to focus on here occurs along the electron transport chain. And the electron transport chain is what’s involved in a chemical reaction sequence of moving electrons from one complex to the next. Okay, from complex I to II, III, IV, for example, with the end result of making water and accumulating protons within the inner membrane space.
So as we’re moving electrons down this chain reaction, we’re getting protons that are being pumped into this inner membrane space. So you’re getting an electrochemical gradient effect within the mitochondria, within the electron transport chain, between the matrix and that inner membrane space.
And so what’s interesting is we get these hydrogen ions—or these protons—that accumulate over top of this ATP synthase complex, and then they move through these chambers. And that movement effect creates a rotation of these oval-shaped protein complexes that basically bring together adenosine diphosphate and inorganic phosphate to make our ATP.
Now, any one of these complexes is vulnerable to nutritional deficiencies, to chemical toxicity, certainly genetic influences as well.
So cytochrome c plays a critical role—if I can go back here—here is our cytochrome c. Okay, cytochrome c plays a huge role between complex III and complex IV of the electron transport chain.
When the inner mitochondrial membrane is disturbed or complexes are not working or the system breaks down, for example, there can be a release of cytochrome c from its placement within the inner mitochondrial membrane. It can leak into the cytosol and trigger what’s called cell death—or apoptosis.
So here is our cytochrome c.
Okay, notice we’ve got complex I embedded across the inner mitochondrial membrane. We’ve got complex II that’s on the inner side. We’ve got complex III that goes all the way across, complex IV that goes all the way across, and complex V—also called our ATP synthase—that goes all the way across.
But strategically, the cytochrome c, which is involved in electron transfer between complex III and IV, sits on the outer edge. And so if we get a breakdown of the inner mitochondrial membrane, okay, or we’re getting disruption of the complexes, this cytochrome c gets expressed out of the mitochondria.
And the outward expression of cytochrome c interacts with enzyme systems called caspase. And there’s different sequences of these caspase enzymes, but the end result is it leads to cell suicide or apoptosis.
Okay, so basically it’s a signal to the cell that we’ve got a problem in the mitochondria, and we need to basically commit suicide. That’s the end result—and that gets triggered by cytochrome c as a normal part of cellular biology.
Well, many of the mycotoxins are actually known to disrupt the mitochondria. So zearalenone, for example—sometimes abbreviated ZEN or ZEA, so I use both—is produced by Fusarium mold. So this is a mold that actually can mimic estrogen or it can have estrogenic effects, so it can really disrupt reproduction, for example, conception, ovulation, and even fetal development.
It has negative effects in the gut as well. But in the context of mitochondria, ZEN or ZEA or zearalenone can damage the mitochondrial membrane. Okay, so it’s basically damaging the mitochondrial membrane potential. So it’s damaging or altering or affecting the electrical gradient effect between the outside and the inside components of the mitochondria. It can also generate reactive oxygen species, for example. All of that can then lead to an expression of cytochrome c.
Ochratoxin, which is linked to Aspergillus mold, is a very potent nephrotoxin, so it’s potent—negatively—to the kidneys. Now, it can also have effects on other organ systems, in the brain as well as the liver. And it too can disrupt mitochondrial activity.
So ochratoxin has a lot of different toxic effects: hepatotoxic, nephrotoxic, immunotoxic. It’s carcinogenic, for example. Mitochondrial dysfunction by lipid—or by lipid peroxidation—so basically oxidizing lipids within the cell membrane. Okay, and so again, outward expression of cytochrome c causing apoptosis. So basically another triggering mechanism for cell suicide.
Now this was an interesting article—came out in 2014—looking at different aspects of ochratoxin toxicity. So in this particular article, they talked about how primary bile acid biosynthesis is compromised. Okay, so that is now linking phase two as well as phase three liver detoxification, as well as disruption of cytochrome P450. So that’s actually linking phase one.
They even went into looking at how ochratoxin can disrupt aspects of methylation and other signaling mechanisms with regards to liver function. So this was particularly looking at liver toxicity.
So if we think about what this paper was mentioning, it’s mentioning that ochratoxin can have a negative influence on phase one. So phase one is what is involved in the initiating chemistry in converting lipid-soluble compounds and starting to move them into phase two.
Now, there’s always going to be an intermediary phase, and this is a potential area of vulnerability for a lot of people—if they are deficient in many nutrients as well as antioxidants—because the chemistry is set that you’re going to actually, in many cases, get an increase of reactive oxygen intermediates, which could cause secondary tissue damage because of free radical formation. That’s why we need a robust, healthy diet—antioxidants—to help buffer against that.
But this paper also talked about how bile formation can be compromised, which links us to what’s called glucuronidation in phase two, as well as methylation.
Now, you could pick apart and look for research into the chemistry of mycotoxins that could affect almost any of these different pathways. We just don’t have the time. You can certainly do some of that research on your own, and this might help give a bit of a head start into kind of how—some things to consider or look at.
Now this was another paper that came out in 2019 looking at ochratoxin-induced hepatotoxicity and the effects on phase one and phase two. It gets fairly complicated, so I’m just going to focus on a few interesting areas here so that we’re not running too long.
But as you can see here, it says ochratoxin triggered oxidative stress as demonstrated by glutathione depletion. So that is going to affect phase one, phase two, as well as increase reactive oxygen species. Well, that could damage cell membranes, damage cellular components, damage the nucleus, as well as the mitochondria.
And then something called malondialdehyde—I’m pronouncing that correctly—I just want to focus on that real quickly.
Aldehydes are chemical compounds that have a carbon double bonded to an oxygen with a hydrogen. And there’s all kinds of examples of aldehydes.
Much of our phase one liver detoxification is meant to deal with different types of aldehydes that we come in contact with naturally through our diet, that get produced as byproducts of our own metabolism, or we come in contact with exogenous compounds like drugs or chemicals or whatever.
Aldehydes by nature are reactive, and they can damage DNA themselves or generate reactive oxygen species, or damage protein, and damage even mitochondria. Okay, they can even deplete glutathione.
And there are different populations of people who have—I guess I should say genetic variants in their aldehyde detoxification enzymes, for example—where they may not handle certain aldehydes that get generated, like from ethanol or alcohol consumption.
It turns out in autism there are individuals who tend to have a weaker aldehyde detoxification system. So basically their bodies don’t handle aldehydes all that effectively.
In fact, this particular paper—if you want to look it up—is very interesting, talking about the pivotal role of aldehyde toxicity in autism.
So simply ethanol. Okay. So ethanol as an alcohol gets converted into acetaldehyde. And it occurs through the actions of alcohol dehydrogenase, and that requires certain cofactors like zinc and NAD to function.
Acetaldehyde should get converted into acetic acid through the actions of acetaldehyde dehydrogenase 2, again through the actions of NAD.
Now, you can have polymorphisms in any of these enzyme systems, for example. Acetaldehyde, from an alcohol standpoint, is likely what’s manifesting or gives you those symptoms of—you had too much to drink: facial flushing, nausea, rapid heartbeat, for example.
Okay, so that’s kind of an acetaldehyde effect. But again, it’s an aldehyde that has that carbon double bonded to an oxygen with the hydrogen coming out the other end. So these are all dealt with primarily through phase one.
I mentioned before that in the presence of other infections it can accentuate some of the toxicity effects of some of these mycotoxins.
And this is just an example of things that we’ve talked about before. And if you currently run organic acid tests, I know you’re going to be familiar with the arabinose.
Okay. Well, it turns out arabinose, as a chemical reflection of invasive Candida at the mucosal lining in the digestive tract, is an aldehyde. So it’s one of the other potential aspects of Candida toxicity.
So again, many people who have mold exposure many times also have a Candida problem—not in every case.
It’s also known that many of the mycotoxins are immunotoxic, which means they have immune-dysregulating properties which can influence the immune system’s ability within the digestive tract to deal with other opportunistic organisms like Candida and sometimes other bacteria.
So it turns out that yeast will take glucose and convert it into ethanol. Okay, so somehow our body has to deal with that. Well, it’s very interesting that the step before ethanol production from a yeast cell is the production of acetaldehyde.
So again, you always sometimes have to think of additional burdens that might be occurring in a given patient in the presence of these exposures.
So where is this going? Well, multiple exposures—or just different types of aldehydes—and the way that they can occupy phase one, those P450 enzymes, for example, and also the inability to activate or engage the P450 system and the potential accumulation of even just something like acetaldehyde generates reactive oxygen species.
These things can have a negative influence on polyunsaturated fatty acids, lipid oxidation, lipid peroxidation. And we get the production of malondialdehyde—another aldehyde—that causes liver damage.
So not everything from a mycotoxin, fungal standpoint is going to have a direct line at toxicity. It just may be affecting other systems that get out of balance that then lead to downstream negative effects, whether that’s the generation of oxygen radicals, hydroxyl radicals, for example.
All of this stuff has a cumulative effect potentially in any given patient.
Let’s come back to trichothecenes. So these trichothecenes are a large family of fungal metabolites—right—these mycotoxins. And there’s different molds that produce trichothecenes.
So the most common would be Fusarium as well as Stachybotrys. Okay, Myrothecium species—you know, Spicellum myces is how it’s pronounced, Cephalosporium, for example.
Stachybotrys likes to grow in damp indoor environments where there’s a lot of water damage. Fusarium can also be a mold that takes advantage of water-damaged building material, but it can also be found in many different types of foods—barley, corn, oats, for example, wheat.
Poisonous mushrooms—I can’t remember the name of it—can produce roridin E and verrucarin, for example.
So these trichothecenes actually have a very interesting chemical structure. Some of them are called macrocyclic. So this—it has this additional kind of expanded ring structure.
So we can see that roridin E, verrucarin A, and satratoxin H are macrocyclic. T2 toxin, which is a common toxin that will be measured in the updated MycoTOX profile from Great Plains, is a common contaminant of food and it’s called a non-macrocyclic—so it doesn’t have that expanded ring.
But one of the key aspects you’ll notice in all of these trichothecenes is this epoxide ring.
Okay. So that exists in all of these mycotoxins—whether it’s macrocyclic or not—at least in this example.
So, what’s the big deal? Well, this epoxide configuration—if I go back—well, here it is right here. From a chemical standpoint, this triangular reaction with the oxygen and single bonds to carbon is very unstable. It’s very strained chemically.
So the way you can think of it is—it sort of takes a lot of—if I’m describing this right, I’m not an inorganic chemist or organic chemist—but a lot of chemical energy or chemical activity to kind of keep this thing together. So they’re highly reactive.
So this reactivity, unfortunately, in biological systems is not good, because it means it can react with different cellular aspects—even the DNA, RNA, for example.
Things called nucleophiles—nucleophile means nucleus-loving—so nucleophiles provide electrons for creating new chemical bonds.
So it turns out that the epoxide, in its high reactivity, will draw in nucleophiles. Some of the things called hydroxide ions or thiols—also called sulfhydryls—okay, to try to neutralize or interact with these epoxide structures.
So this is what makes these trichothecenes so reactive.
So we know that they can do a lot of damage in very high amounts.
If we think of that, a very common thiol group is one that actually exists on glutathione. So glutathione can be very important in the detoxification—or attempt at neutralization—of some of the toxic effects of these mycotoxins like trichothecenes.
But that also means that it puts a lot of strain biochemically in the body to maintain glutathione levels.
You think about where glutathione is getting produced—it’s coming off of the methylation cycle through a pathway called transsulfuration. Anytime there is the existence of these mycotoxins or other toxic compounds in the body, it’s putting increased demand on glutathione reserves.
So this is where patients can get into trouble in depleting glutathione in the presence of various toxins.
And then, of course, the downstream effects of glutathione deficiency just put a lot of cellular components at risk—including the mitochondria.
So the liver and its detoxification—just as an overview or a recap—right, protects us or tends to protect us from various compounds by its ability to convert fat-soluble compounds into water-soluble metabolites, to get rid of these things through our bile or through the kidneys.
And so the complicated chemistry that occurs within phase one—oxidation, reduction, hydrolysis reactions—and phase two, which a lot of them are conjugation reactions, transforming chemicals into a less toxic compound, all of these things are acting upon these different functional groups that are situated on these different compounds.
So an aldehyde, for example, is a functional group from an organic chemistry standpoint.
Now, remember also that the steps between phase one and phase two is a vulnerability area where you can actually increase oxygen radicals and free radicals. This is why we, as well as our patients, need to have the healthiest diet possible to try to prevent that from happening.
So fundamentally, it comes down to the nutrients from our food. Okay—vitamins, minerals, amino acids, antioxidants—are necessary for proper, not only just proper liver function but detoxification function, which is a huge role obviously of the liver.
So phase one—right—we’re converting things from a water-soluble form, activating a lot of those P450 enzymes. And so again, we need robust nutrition—so B vitamins, choline, vitamin C, magnesium, other minerals.
Broccoli is a food that has been shown to be helpful for phase one. Brussels sprouts, cabbage, citrus fruits, grapefruit juice.
Now grapefruit juice extract can have a diminishing or slowing down effect on phase one. And so that becomes important in certain patients who are on different kinds of medications, for example, because the concern might be that grapefruit juice could actually increase the ongoing circulation of a medication that might be problematic.
Phase two—we’re now moving into that transformation into a fat-soluble form. This is where a lot of those conjugation reactions take place. So we need good sulfur amino acids, methylation support, for example.
So—and again—similar vitamins: B5 is important for what’s called acetylation. B12, folate—important for methylation.
Glutathione plays a big role in phase two liver detoxification. But we can’t discount the fact that even glutathione could be beneficial in phase one as well as the intermediate phase—just protecting against a lot of free radical formation.
Phase three is interesting—it often gets overlooked or not well recognized. But this is that transportation of these detox products into the biliary system. So we need good bile flow.
So phosphatidylcholine is important for bile production. Calcium D-glucarate helps support glucuronidation, which honestly is kind of a segue between phase two and phase three.
And then there are different herbs—a lot of the bitter herbs: artichoke, dandelion, peppermint—can help stimulate bile production and bile flow within the liver.
So these are example slides here—supplements of phosphatidylcholine. This comes from Designs for Health. I mean, there’s other companies that have phosphatidylcholine too.
But this is a nice remedy that helps to enhance bile secretion and flow. So it’s very supportive of phase three. It keeps the bile liquid, it helps prevent against gallstones. Also helps very much in the stimulation of small intestine and large intestine activity with regards to bowel movements.
So a lot of people will take one to two capsules or soft gels in the evening—not only for liver support in general, for bile support—but also for digestive support with regards to bowel movements in the morning.
LVGB Complex—again, this is just an example. There are other companies that have similar products. This is really, again, another support for phase three. It has some phase two components or just general liver support components with regards to things like milk thistle and eleuthero.
So ox bile, artichoke extract, beet powder—a lot of times this combines nicely with the phosphatidylcholine for just general liver support with regards to phase two, phase three.
And then this is just an example—there’s these different types of bile-stimulating herbs. We’ve had some patients do well where they actually wake up in the morning and they’ll have, you know, a decent glass of warm water. Drink that first, and even just to put something like, you know, 10–15 drops of this in the warm water in the morning—just as a stimulant for liver bile production as well as gallbladder movement of bile—all with the idea that it’s going to help support or initiate the aspects of detoxification in the early morning hours.
Which is important, because one of the things is we want to make sure that people are having normal bowel movements. Because trying to initiate a detoxification program in a patient that’s constipated is problematic.
So the aspect of bile is very much linked to glucuronidation, for example, which is a component of phase two and certainly has aspects that transfer over into phase three or bile excretion.
So aflatoxins, the T2 or H2 toxins—which are trichothecenes—the ZEA or zearalenone, for example, are all detoxified by glucuronidation.
Watch out for constipation. Okay, we know that a lot of people are constipated and that could be a problem. So again, we can have—you know—we can induce liver function and detoxification, but in a constipated patient, that’s real problematic because you dump the toxins into the gut and then they have nowhere to go and they end up getting a lot of them reabsorbed, which is certainly problematic.
So again, you know, Designs for Health—this is just some magnesium hydroxide with triphala. It’s a nice combination for normal bowel function. A lot of patients who have constipation issues will do a capsule of this along with some phosphatidylcholine, for example, drink a warm glass of water with maybe a lemon squeeze in it or maybe some bitter herbs to help stimulate bowel movements, and this can be tremendously helpful.
Fiber is also very important. We know that fiber is necessary for bulking of stool.
So the two most common causes of constipation in North America are lack of fiber and dehydration.
I use a lot of this product from New Beginnings Nutritionals. This PureLean Fiber works well as a fiber supplement. New Beginnings also has a lot of other products for liver support and magnesium as well, which can also be used—like magnesium glycinate, for example, can be often used just for magnesium purposes.
Hydration is key. Right—people who are dehydrated tend to be more constipated. So this is also a very important aspect for normal bowel function. But it’s going to be an important aspect of detoxification.
Remember, there’s an old—and I can’t remember if it’s a… I can’t remember where I heard it—but there was a comment: “The solution to pollution is dilution.” So keeping our body hydrated is really important.
And this is clearly important when we think about kidney function.
So let’s segue now over and talk a little bit about the kidneys.
And we could spend hours just talking about the anatomy and the physiology of the kidneys. They’re very complex in what they do, just like so many other aspects of our body. But we often sort of take these things for granted until they don’t work.
But the kidneys are vulnerable to these toxins too. So it turns out that many of these mycotoxins that we’ve been discussing attack the kidneys—whether they cause mitochondrial degeneration, whether they cause damage within some of the tubules, whether they cause vascular swelling, or they cause degeneration of the epithelial lining—it can all lead to kidney dysfunction.
So the basic structure of a nephron—I’m not going to go through all of these things because we don’t need to, it’s too complicated. But just think of the nephron as the filtering mechanism of the kidney.
And so, a couple highlights: the distal convoluted tubule that you see circled here—it has a vital role in the secretion of various electrolytes, particularly the hydrogen ions as well as nitrogenous wastes. So it’s a part that is very much involved in the removal of toxins.
So if you just remember that—if you disrupt the distal convoluted tubule because of a mycotoxin, now the kidney is already compromised in its ability to start getting rid of nitrogen or nitrogenous waste compounds and other toxins.
The proximal convoluted tubule—okay, this deals approximately with about 80% of the filtrated water, nutrients, electrolytes, small proteins, and albumin molecules that are reabsorbed from the proximal convoluted tubule.
So if it’s taken out, now we’re going to be compromised in our ability to reabsorb certain nutrients, small proteins (which we need to act as colloid substances within our vasculature), our electrolytes—albumin gets compromised.
And that has effects within our vasculature, for example. It has aspects within regulatory mechanisms between the extracellular and intracellular aspects of our cells.
So again, damage within the kidneys is going to have effects within our body that can affect different organ systems as well.
The loop of Henle is a place that is very much involved in the regulation of sodium, chloride, and water. So if we damage the loop of Henle—and there’s different aspects of it—now we’re going to compromise fluid hydration as well as compromise chlorine, chloride, and sodium.
If we affect hydrogen ions, that’s going to affect our pH. If we affect sodium, chloride, and small proteins, other aspects—that’s going to affect not only pH, but the electrolyte balance in our body as well.
So again, very simplistic overview. But unfortunately, the downstream effects of kidney damage are not good.
In fact, this is an image here—this was a paper that was specifically looking at T2 toxins, which is a trichothecene. And I wanted to just show that it can lead to necrosis—so basically necrosis of these tubular cells, these renal tubular cells.
And just think of these renal tubular cells as part of the proximal, the distal convoluted tubule, the loop of Henle—all of those cells that are involved in hydrogen regulation, sodium regulation, reabsorption of proteins, etc.
Also notice that all of these cells require mitochondria. Right? So the mitochondria within the kidneys can be affected, which can then affect the filtering mechanisms in the kidney too.
But I want to just touch on one aspect of kidney disease. And that starts to bring in aspects of the immune system.
So, in necrosis—it should say in what’s called apoptosis, or apoptosis as it’s pronounced different ways—when a cell starts to break down, it can express something called DAMPs: danger-associated molecular patterns.
Now, typically a DAMP, when it is overexpressed, can lead to uncontrolled cell death.
In a proper formation or sequence in which a cell is initiated or triggered to commit suicide, the DAMPs that are linked—and DAMPs are basically inner components of a cell that are normally hidden away from the immune system—the DAMPs essentially are hidden or they’re sequestered. And we get a normal breakdown of the cell that then gets engulfed by a macrophage, and then that essentially gets cleared from the body and we do not get an abnormal immune reaction.
So apoptosis essentially is a programmed cell death response where the cell gets taken out of circulation. It’s not breaking down and spilling its guts and spilling its contents, creating damage in the area that then triggers an adverse immune reaction and then subsequent inflammation. So that’s basically the bottom line to that.
But remember that trichothecenes can lead to necrosis. When we have cells that are necrotic, they’re not being cleared quickly enough, or the breakdown is so fast and so robust that the internal contents of a cell—which are normally sequestered away and hidden from the immune system—all of a sudden get expressed outside the cell.
And within all of our bodies, we have different receptors that recognize these different cellular components—or sometimes components of a microbe, for example.
But if this was our own body and our own cells, for example, all of a sudden, we now engage the immune system in a different type of response.
And the problem is, in an apoptosis situation, the cell that dies—that could be our own cell—gets taken out by a macrophage, and then it’s removed, and nobody knows the difference. Okay? The immune system basically stays quiet, and everything is in balance.
But in necrosis, we do start to trigger immune responses that don’t work really in all cases to our benefit.
So here’s a classic example: we have things that are called polymorphonuclear sites, and these are different cells that have different granules—so eosinophils, neutrophils, mast cells, for example.
Monocytes are part of our innate immune system. So our polymorphonuclear sites—though part of our innate immune system as well—sit in our tissue.
And just think about the liver or the kidney. So just imagine this is a slide that sits on top of the kidney or sits on top of the liver—we’ve got macrophages which are sitting within those tissues. And we’ve got monocytes that are circulating throughout the bloodstream that get triggered to move into an area where there’s a problem.
You know, in some cases, these monocytes can go right ahead and transform into a macrophage as well. So we usually have resident macrophages, and then we have monocytes that become macrophages that add to that army of macrophages.
If we have an infection or we have damage or we have necrosis that is occurring within tissue, neutrophils, for example, can get pulled into the tissue space. So if that’s the liver or the kidney or elsewhere, the neutrophil will come in, and it will engulf or attempt to deal with that problematic cell or that pathogen.
So it will engulf it, and it becomes what’s called an apoptotic PMN—or an apoptotic neutrophil—basically it’s waiting to be taken out by a macrophage.
So there’s chemical signals that get sent to make all this happen.
So if the macrophage comes over and engulfs this neutrophil, okay, no harm done. It’s removed from the system, and we’re good to go. The immune system isn’t hyperreactive. We don’t have inflammation or chronic inflammation.
The problem is if we’ve got issues that might be happening within the macrophages, or we’re getting degeneration of cells too quickly, or these apoptotic neutrophils aren’t getting removed…
Well, it turns out, over time—usually about 6 to 11 hours—it takes for an apoptotic neutrophil to get cleared out of the system. It too can start to break down, and as it breaks down, it starts releasing its internal contents. It starts spilling its guts—its guts into the tissue space of that organ.
That then just triggers more activity, which then triggers more inflammation.
So there’s a whole sequence of events that have to happen in order to normally remove a cell that has engaged a pathogen—or a cell that has been damaged.
And if it doesn’t do it quickly enough, we now are stuck in a state of chronic inflammation. So what’s called “failure of resolution.”
If we take this back to the fundamental level of the organic acid test, we know that the organic acid test evaluates for the exposure to different types of mold.
So markers 2, 4, 5, and 6 indicate gut colonization of Aspergillus within the digestive system. Tricarballylate is an organic acid marker that is reflective of Fusarium mold. These are not mycotoxins. These are organic acids off of the organic acid test.
At this point, I don’t know what this person’s mycotoxins look like, but I have a suspicion that—at least in the presence of Aspergillus or Fusarium—that I could be looking at ochratoxin, gliotoxin, as well as maybe some of the trichothecenes.
Okay, so that’s where the organic acid test comes into play.
Well, we also know that Candida—which is what’s producing, or I should say, arabinose gets produced because of the invasive nature of Candida—and Aspergillus can produce oxalic acid, another marker found in the organic acid test.
Well, Aspergillus, Aspergillus niger, for example, in this example, through its Krebs cycle produces citrate or citric acid, which then comes out of the cell and gets acted upon by an enzyme—it’s actually, here’s the enzyme, well here’s the enzyme right here—it’s citrate gets acted upon by an enzyme called oxaloacetate hydrolase, and that makes oxalic acid.
So it turns out that Aspergillus can actually make oxalic acid by compounds from its own Krebs cycle. It then gets pumped out of the cell, and that’s how we accumulate oxalates in relationship to Aspergillus—whether it’s occurring in the sinuses, whether it’s occurring in the gut, whether it’s occurring in the lungs, or wherever that Aspergillus is sitting—it can produce oxalate.
So, what does this mean in relationship to cell function?
Well, it turns out that oxalate can bind with calcium to make calcium oxalate crystals. There was a paper that was looking at what were called monohydrate and dihydrate crystals in relationship to oxalate.
Oxalate crystals can cause reactive oxygen species. They can trigger membrane damage within the cells, including the mitochondria.
And remember, the mitochondria—by damaging its inner mitochondrial membrane, maybe even the outer mitochondrial membrane—but basically damage of the mitochondria can cause an outward expression of cytochrome c, which is a trigger for those caspase enzymes that are sitting within the cytosolic fluid of the cell. Those caspases get activated. That is a chemical reaction to trigger cell suicide.
All right, so these are just the calcium oxalate monohydrate, calcium oxalate dihydrate. Okay, they get taken into the cell, and they can generate reactive oxygen species. The reactions can even damage the nucleus of the cell, for example. Or they can damage the mitochondria.
Okay, again—damage the mitochondria—we get an outward expression of that cytochrome c. That triggers apoptosis.
Now, if you think about it—if that sequence occurs in a normal, somewhat regulated fashion, and all we’re getting is apoptosis, then we shouldn’t be generating a lot of adverse immune reaction or even a lot of inflammation.
The problem is when it happens very quickly, very robustly, before the immune system has a chance to clear these things out.
And there’s actually another aspect of ptosis called necroptosis. And some of this is—I don’t know how long some of this has been around, as far as when it was discovered—but necroptosis is another type of cell death response. It’s called a regulated necrosis effect.
So in theory—okay—because it’s regulated, it shouldn’t generate a lot of inflammation.
Okay, but it’s not the same exact cellular sequence of just regular apoptosis.
So some of the literature you read, depending on how robust this is happening or how quickly it’s happening, it is certainly possible that inflammation can be triggered because of necroptosis as well.
And certainly like anything with any organ system—how much is happening, how quickly the cells are being affected, how quickly the immune system can respond—are all determining factors in the kind of collateral damage effect that you will get.
But what is crystal clear is that oxalates can cause mitochondrial problems.
And the mitochondrial dysregulation can lead to—whether it’s just necrosis or apoptosis—you’re going to get problems that happen in these organ systems. And this is happening in the liver, it’s also happening in the kidneys, and it’s happening throughout the body.
You could almost think—although I’m not going to say it—but you could almost think of oxalate as a type of mold toxin.
I’m not going to call it a mycotoxin, but because clearly you can get oxalates from other reasons, right? You can get it from your food, and it can come from, you know, genetic factors and whatnot.
But it’s another aspect of how mold exposure could cause problems in the body—not specifically by a classic mycotoxin like trichothecene or ochratoxin—but by secondary influence of just oxalate accumulation.
So I’m going to finish up and recommend you read a great blog article that just came out—it actually was great timing in coordination with my lecture.
This comes from Lindsay Goddard, who’s a nutritionist consultant, registered dietitian at Great Plains Lab, and she does great work—great article.
If you want to read this article—which I’d encourage you to do—as well as previous posts on blog articles from Great Plains, just go to their website and look under the resource section and you can pull up their blog site.
She actually wrote an article on the often-forgotten part of detoxification, which is the kidney.
And actually, she did such a great job in this article—I actually just took a screenshot and kind of modified it down for this slide. So this was actually taken from Lindsay’s blog post talking about just some basic things that you can remember for your patients with regards to basic kidney functions.
So again—staying hydrated, right? Keeping things flushed. The solution to pollution is dilution.
And again, we’re not getting into—obviously in this lecture—the management of people with, you know, chronic kidney disease, for example. That obviously is a more complex discussion.
But regulating sodium and phosphorus, for example—okay—because excess amounts can cause imbalances in the kidneys.
Movement—so I’m huge on exercise. Lindsay points out that just movement of the body—walking, yoga, whatever: exercise, bicycling—is very important to keep things moving.
Okay, various functional foods—many of the healthy foods we talk about that are often important from an antioxidant standpoint help to decrease inflammation, and also can be supportive for kidney function.
And N-acetylcysteine—as she states—can be important for glomerular filtration effects within the kidneys.
And then certain herbal compounds—now again, that could be a whole other discussion on certain herbals being sort of stressful for the kidneys, for example. So, you know, that may take some additional research.
But check out Lindsay’s blog post and some of the back posts that are available on that part of the site.
So real quickly I just want to finish on one final note here—that it’s always in my view—and I sound like a broken record probably because I’ve said this so many times—but my recommendation is, when it comes to testing: don’t just do the MycoTOX profile.
Yes, it is an important test to do. It’s the only way of evaluating for the existence of mycotoxins. But it should always be paired with the Organic Acids Test—if the Organic Acids Test has not been done.
Because there are so many other aspects in the Organic Acids Test that are important to pick up on—from mitochondrial activity, bacterial infections, etc.—that may coincide with things on the MycoTOX or are being influenced by the MycoTOX profile.
Okay, so that is the lecture here for this topic. I hope you found that helpful.
If you are a healthcare practitioner, we actually have a website called Functional Medicine Clinical Rounds. This is a membership site for healthcare practitioners that you can join. You can have one-on-one consults with myself, my partner Dr. Tranchitella. We also have some educational material on this site as well. We can go over labs, we can talk about cases, troubleshoot—a great website resource if you’re interested.
If you are interested in any of our courses through Integrative Medicine Academy, we’ve got courses on autism, on functional medicine, on toxicology, on mold, on organic acid testing.
Go to integrativemedicineacademy.com. We actually have a new Functional Medicine Mastery course that will be starting here shortly.
So for more information, you can go to Integrative Medicine Academy and check out our different courses.
There’s a website called Lab Test Plus that does provide access to Organic Acids Test, MycoTOX profiles, many of the other labs from Great Plains. Every one of these labs will come with a written review of relevant findings, including those on the MycoTOX profile.
So you can get more information at labtestplus.com or you can email questions to labtestplus@gmail.com regarding accessing lab tests through this website.
Okay everybody, and there—there’s my information. If you are interested in consulting with me privately, my website is mysunrisecenter.com, and then there’s the email and phone number.
So once again, I want to thank Great Plains for sponsoring these monthly webinars. I always enjoy doing them. I hope you found this webinar informative.
And we will see you again next time. I’m Dr. Kurt Woeller. Thank you.