“Should I eat eggs?” “Are eggs good for me?” “Do eggs have a lot of cholesterol?” If you are a healthcare professional, you’ve probably heard at least one of these questions. Or if you’re a health-conscious consumer, you’ve probably thought about these questions or asked them yourself. With the slew of research regarding cholesterol levels and its effect on health, it’s understandable why these questions arise. The biggest concern with cholesterol is having too much. High levels of cholesterol have repeatedly been linked to poor cardiovascular health outcomes. But what about low cholesterol? Are there situations that may warrant a higher level of cholesterol? This post aims to sort through some of the research linking cholesterol levels and neurologic conditions. On your search to identify total cholesterol levels, look to the Advanced Cholesterol Profile offered by Mosaic Diagnostics.
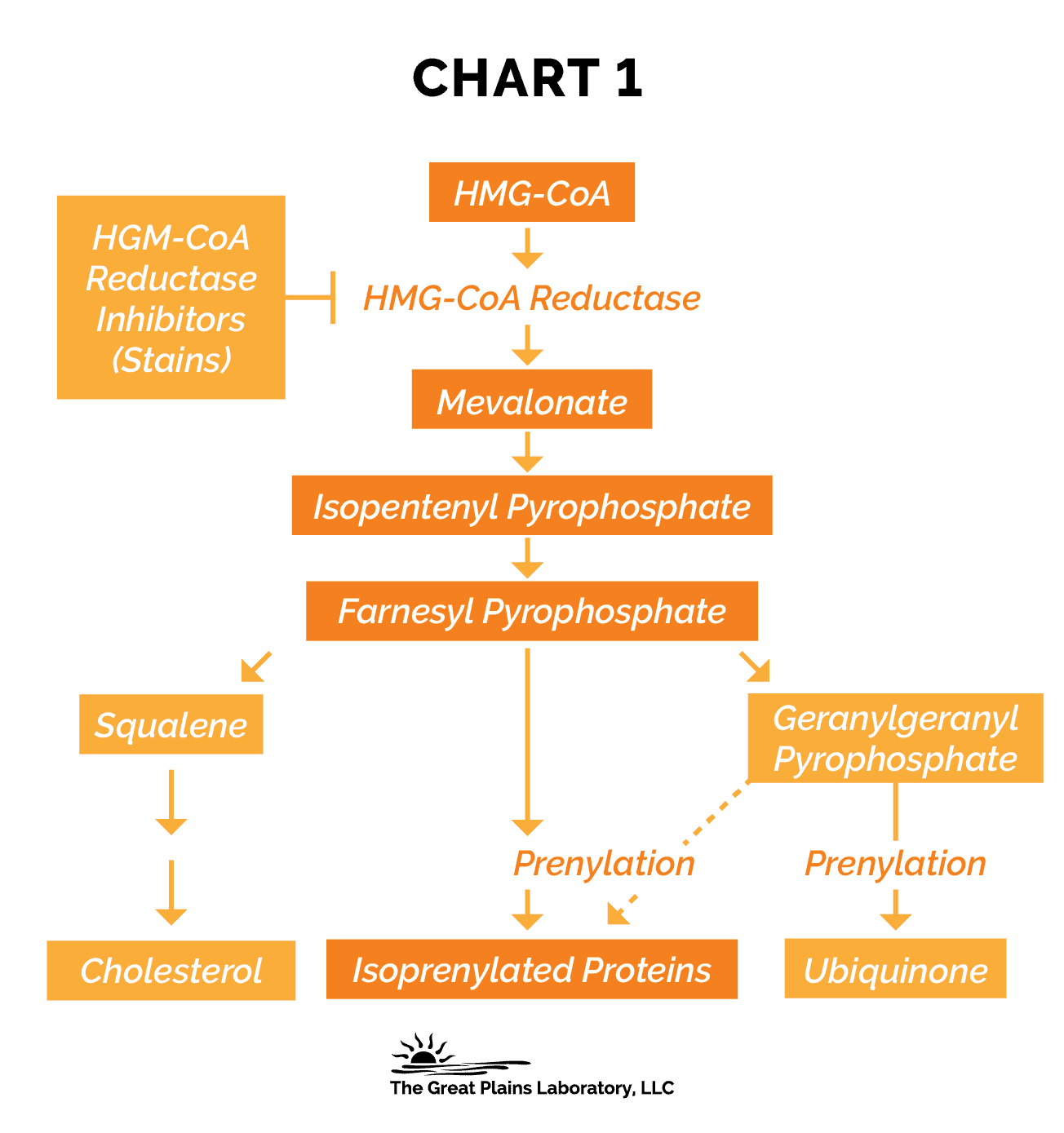
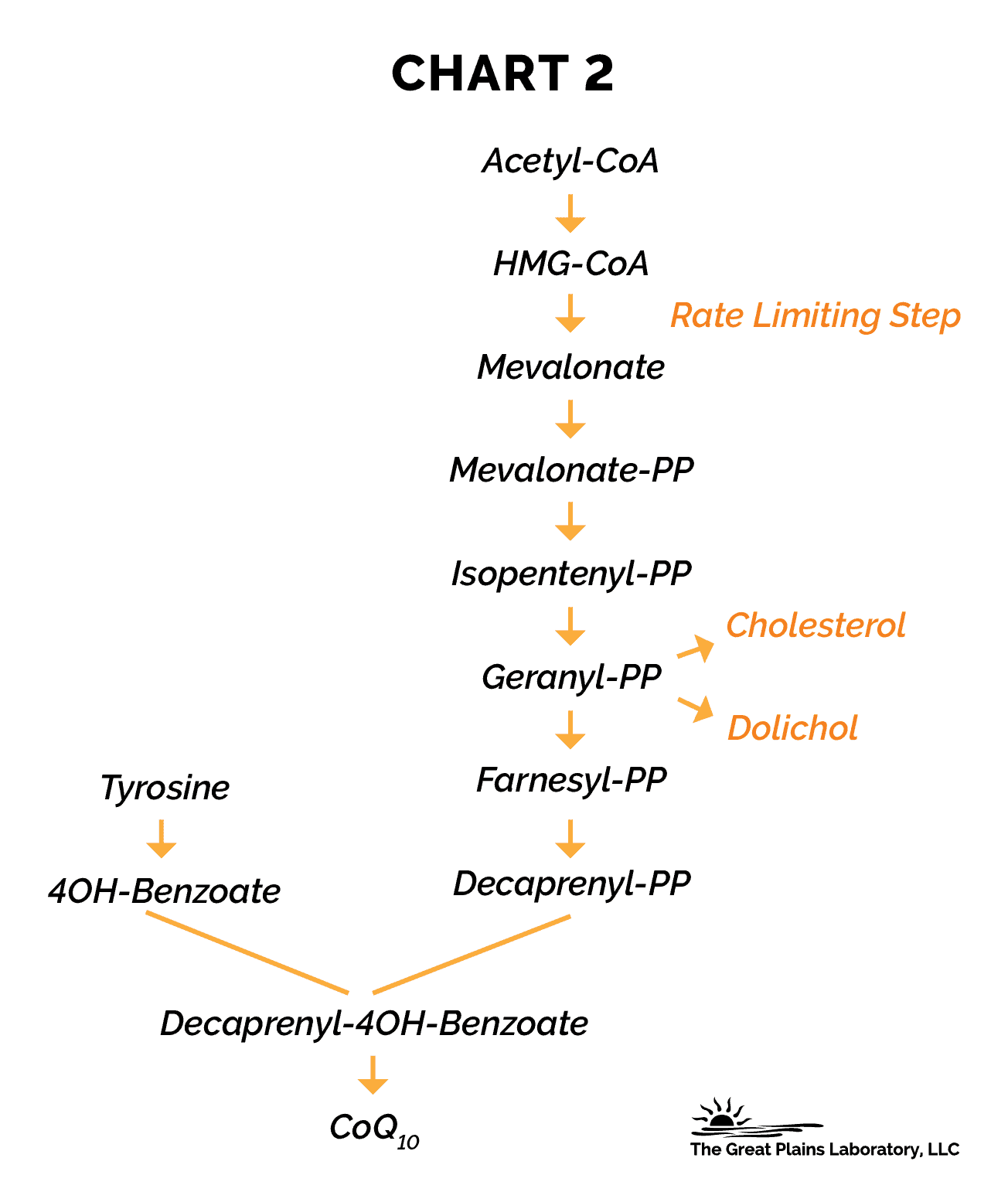
In the human body, cholesterol is synthesized through a complex series of biochemical reactions. Acetyl CoA molecules are converted to HMG CoA via a series of thiolase and HMG synthase enzymes regulated by the supply of cholesterol (7, 8). HMG- CoA, also known as 3-hydroxy-3-methylglutaryl coenzyme-A (4), is then reduced by HMG CoA reductase to create mevalonate. This is the rate limiting step in cholesterol synthesis (1). This enzyme is an important hub in cholesterol and CoQ10 synthesis. It is also heavily studied as the main enzyme inhibited by statin drugs. After HMG CoA is reduced and mevalonate is produced, a series of reactions creates Farnesyl-PP. This is the branching point for cholesterol synthesis or CoQ10 synthesis (1, 4). From here, farsenyl-pp can become squalene that then becomes cholesterol or geranylgeranyl-pp to become ubiquinone (CoQ10) (10). Since the regulatory enzyme in this process is HMG CoA reductase, when it is inhibited by prescriptions or supplements, like statins and red yeast rice, it will cause a decrease in CoQ10 production. This also means cholesterol is lowered. Great Plains Laboratory offers a urinary Organic Acids Test that contains a marker for this enzyme function. This is marker #55 or 3-Hydroxy-3-methylglutaric acid. This is the urinary organic acid for HMG CoA. In the presence of excess in this marker, we know that mevalonate is not being made and the HMG CoA reductase enzyme has decreased functioning. This informs us of a need for CoQ10 supplementation. Information from this marker may also lead you to look at total cholesterol levels, especially in those on statin drugs or anyone presenting with neurologic conditions associated with lowered cholesterol levels.
In the human brain, cholesterol plays an important role. The brain contains 25% of the body’s cholesterol, making it the most cholesterol rich organ (6, 15). Cholesterol is necessary for normal function and is made de novo in the brain tissue (15). Most of the cholesterol is found in the myelin which makes up about half or so of the white matter (11). Cholesterol plays a great role in creating the nodes of Ranvier. These are the periodic gaps in the myelin on the nerves (3, 12). These gaps allow for increased nerve impulse conduction through a process called saltatory conduction, which causes the action potential to jump from node to node (3, 12). In genetic conditions like Smith-Lemli-Optiz syndrome, there is a defect in 7-dehydrocholesterol-7-reductase. This causes cholesterol to be replaced by 7-dehydrocholesterol leading to a common symptom of this condition, intellectual disability (11). This genetic origin of a lowered state of cholesterol synthesis gives rise to stark neurologic dysfunction. So, what other conditions are linked to lowered cholesterol levels?
A common mental health diagnosis has garnered attention when looking into the correlation with cholesterol levels. In various studies, lowered cholesterol levels have been associated with increased diagnosis of major depression. Women with total cholesterol levels less than 160 mg/dl, scores on anxiety and depression scales were at 35% vs women with normal levels only score high at a rate of 19% (17). In psychiatric populations, low levels of cholesterol were linked to major depression, while low HDL-C was linked to suicidal ideation (6). Postpartum depression in a subgroup of depression linked to the development of depressive symptoms in the first 6 weeks post-delivery. Common factors related to PPD are troubles sleeping, preterm birth, infant gender dissatisfaction, prenatal anxiety, fear of labor, and mode of nursing with formula or breast/formula feeding. Along with these factors, lowered median serum levels of TC and HDL-C were associated with increased depressive symptoms and suicidal ideation in this population (14). Anxiety, although not as studied, has shown an inverse correlation with TC levels (16). This is important as anxiety and depression often occur simultaneously.
In relation to aggression and violence, low cholesterol has been researched as a potential biomarker. Unfortunately, most of the research focuses on the mental health community diagnosed with schizophrenia and/or bipolar disorder. These studies haven’t shown a strong enough correlation to use total cholesterol as a biomarker for aggression and violent suicide, but non-statistical low levels were seen (5). In the few studies completed on humans and non-human primates, there was a correlation between lowered total cholesterol and violence (16). Though this isn’t strong enough to use as a biomarker, it should be evaluated as a contributing factor along with other underlying causes.
In the pediatric world, the diagnosis of Autism Spectrum Disorder (ASD) has significantly increased. According to the CDC, 1 in 44 children are diagnosed with being somewhere on the spectrum (2). Research has begun to look at the connection between inadequate cholesterol levels and ASD prevalence. Some studies conducted have shown correlations with children on the spectrum having low levels while their unaffected siblings did not (9). Also, maternal and paternal dyslipidemia was associated with offspring with an increased incidence of ASD (9). This may be a strategy to help fertility clients to correct prior to conception as a method of prevention. Other studies have linked an increased ASD risk with genetic conditions associated with low cholesterol like Rett syndrome and Smith-Lemli-Opitz syndrome (13). These correlations and links make cholesterol levels a new and exciting potential biomarker to optimize in the population. Further research would be needed for it to be more of a diagnostic marker. Also, note that ASD was seen in individuals on lipid-lowering drugs, but more commonly in those who were not (13).
With all this information there is a link between low cholesterol and neurologic function. How could there not be? With the brain being made of 25% cholesterol, this substance is quite important. Research is still needed to improve the diagnostic power of TC but in any neurologic condition, it should be assessed. In cases where cholesterol is suboptimal, consider replenishing these levels with food like fatty fish, shrimp, or eggs. After three months, reassess your progress with the client and lab work. Even though more research needs to be completed to make this a household test for neurological diagnoses, TC is a promising piece to various health puzzles.
References
Bank, G., Kagan, D., & Madhavi, D. (2011). Coenzyme Q10: Clinical update and bioavailability. Journal of Evidence-Based Complementary & Alternative Medicine, 16(2), 129–137. https://doi.org/10.1177/2156587211399438Centers for Disease Control and Prevention. (2021, December 2). Data & statistics on autism spectrum disorder. Centers for Disease Control and Prevention. Retrieved March 10, 2022, from https://www.cdc.gov/ncbddd/autism/data.htmlEncyclopædia Britannica, inc. (n.d.). Node of ranvier. Encyclopædia Britannica. Retrieved March 8, 2022, from https://www.britannica.com/science/node-of-RanvierFriesen, J. A., & Rodwell, V. W. (2004, November 1). The 3-hydroxy-3-methylglutaryl coenzyme-A (HMG-COA) reductases - genome biology. BioMed Central. Retrieved March 4, 2022, from https://genomebiology.biomedcentral.com/articles/10.1186/gb-2004-5-11-248Hjell G;Mørch-Johnsen L;Holst R;Tesli N;Bell C;Lunding SH;Rødevand L;Werner MCF;Melle I;Andreassen OA;Lagerberg TV;Steen NE;Haukvik UK; (n.d.). Disentangling the relationship between cholesterol, aggression, and impulsivity in severe mental disorders. Brain and behavior. Retrieved March 10, 2022, from https://pubmed.ncbi.nlm.nih.gov/32681586/Hussain, G., Wang, J., Rasul, A., Anwar, H., Imran, A., Qasim, M., Zafar, S., Kamran, S. K. S., Razzaq, A., Aziz, N., Ahmad, W., Shabbir, A., Iqbal, J., Baig, S. M., & Sun, T. (2019, January 25). Role of cholesterol and sphingolipids in Brain Development and neurological diseases - lipids in health and disease. BioMed Central. Retrieved March 10, 2022, from https://lipidworld.biomedcentral.com/articles/10.1186/s12944-019-0965-zKumari, A. (2017, November 17). Cholesterol synthesis. Sweet Biochemistry. Retrieved March 4, 2022, from https://www.sciencedirect.com/science/article/pii/B9780128144534000078Liscurn, L. (2004, January 7). Chapter 15 cholesterol biosynthesis. New Comprehensive Biochemistry. Retrieved March 4, 2022, from https://www.sciencedirect.com/science/article/abs/pii/S0167730602360174Luo Y;Eran A;Palmer N;Avillach P;Levy-Moonshine A;Szolovits P;Kohane IS; (2020, September 26). A multidimensional precision medicine approach identifies an autism subtype characterized by dyslipidemia. Nature medicine. Retrieved March 10, 2022, from https://pubmed.ncbi.nlm.nih.gov/32778826/Marcoff, L., & Thompson, P. D. (2007, June 5). The role of coenzyme Q10 in statin-associated myopathy: A systematic review. Journal of the American College of Cardiology. Retrieved March 4, 2022, from https://www.sciencedirect.com/science/article/pii/S0735109707010546Meaney, I. B. and S., Björkhem, I., Ingemar Björkhem From the Division of Clinical Chemistry, Meaney, S., Steve Meaney From the Division of Clinical Chemistry, & Björkhem, C. to D. I. (2004, February 5). Brain cholesterol: Long secret life behind a barrier. Arteriosclerosis, Thrombosis, and Vascular Biology. Retrieved March 8, 2022, from https://www.ahajournals.org/doi/full/10.1161/01.ATV.0000120374.59826.1bOrth, M., & Bellosta, S. (2012). Cholesterol: Its regulation and role in Central Nervous System Disorders. Cholesterol, 2012, 1–19. https://doi.org/10.1155/2012/292598Pesheva, E. (2020, August 17). Autism-cholesterol link. Autism-Cholesterol Link | Harvard Medical School. Retrieved March 10, 2022, from https://hms.harvard.edu/news/autism-cholesterol-linkPillai, R. R., Wilson, A. B., Premkumar, N. R., Kattimani, S., Sagili, H., & Rajendiran, S. (n.d.). Low serum levels of high-density lipoprotein cholesterol (HDL-C) as an indicator for the development of severe postpartum depressive symptoms. PLOS ONE. Retrieved March 10, 2022, from https://journals.plos.org/plosone/article?id=10.1371%2Fjournal.pone.0192811S;, O. M. B. (n.d.). Its regulation and role in central nervous system disorders. Cholesterol. Retrieved March 8, 2022, from https://pubmed.ncbi.nlm.nih.gov/23119149/Suarez, E. C. (1999). Relations of Trait Depression and Anxiety to Low Lipid and Lipoprotein Concentrations in Healthy Young Adult Women. Europe PMC. Retrieved March 10, 2022, from https://pubmed.ncbi.nlm.nih.gov/10367605/#:~:text=Conclusions%3A%20In%20healthy%20young%20adult,known%20to%20influence%20lipid%20concentrations.Women with low cholesterol may be at risk for depression and anxiety. Duke Health. (n.d.). Retrieved March 10, 2022, from https://corporate.dukehealth.org/news/women-low-cholesterol-may-be-risk-depression-and-anxiety#:~:text=In%20a%20study%20of%20121,normal%20or%20high%20cholesterol%20levels.