Sidney Baker, MD; William Shaw, PhD
IMCJ Integrative Medicine • Vol. 19, No. 4 • August 2020
Abstract
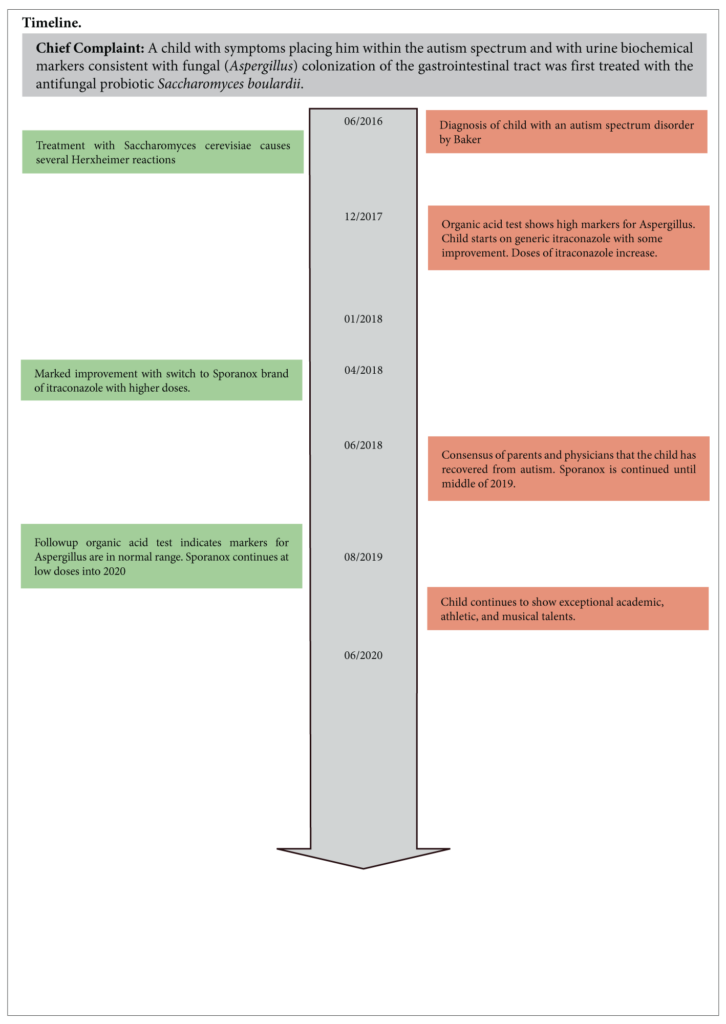
Context: A child with symptoms placing him within the autism spectrum and with urine biochemical markers consistent with fungal (Aspergillus) colonization of the gastrointestinal tract was first treated with the antifungal probiotic Saccharomyces boulardii. A dramatic Herxheimer reaction provided strong clinical indications that mold colonization might be a factor in causing autism in this child.
Objective: The child’s physician (Baker) wished to try a more potent antifungal therapy, itraconazole, in an attempt to reverse the child’s autism since itraconazole is an especially effective agent against Aspergillus species.
Setting: The child was treated as an outpatient by the physician who had first diagnosed the child with an autism spectrum disorder.
Participant: A child with an autism spectrum disorder.
Intervention: The major intervention was increasing doses of the antifungal drug itraconazole. However, the Sporanox® brand of itraconazole gave the best results. The child was monitored twice weekly with liver function tests which remained normal throughout the therapy.
Results: The child had a complete recovery from all the symptoms of autism and in addition developed excellent academic, athletic, and musical skills. The recovery coincided with a marked reduction of urine markers of Aspergillus colonization.
Conclusions: Escalation of the dose of itraconazole resulted in a complete loss of all symptoms of autism over the course of three months. This rapid complete reversal of autism is consistent with several articles proposing mold in general and Aspergillus specifically as a potential major cause of autism.
Introduction
The terms autism or “autism spectrum disorder” (ASD) generally refer to a group of neurodevelop-mental disorders characterized by a broader phenotype, including typical features such as stereotyped or repetitive behaviors, impaired social activities, and restricted verbal and non-verbal communication. Autism effects more males than females: recent epidemiological studies suggest that the ratio in the prevalence/incidence of ASD is in the range of 4–5:1 male: female.1 A trend in male: female ratio of population shows convergence from greater than 4:1 in 2010 to 2012 to less than 3:1 in the year 2013.
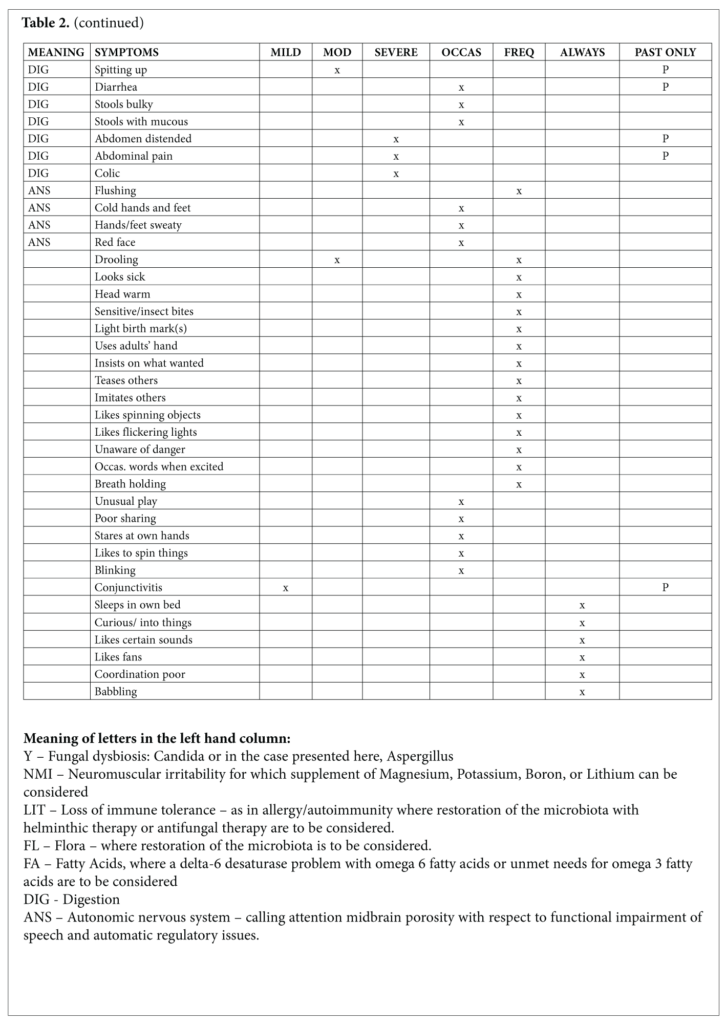
The word spectrum became attached to autism in 1985.2 Spectrum came into common usage around the year 2000 and remains uniquely attached to autism. Parents and professionals find themselves very differently placed: the former lost in a space that lacks the specificity expected from a diagnostic label and the latter welcomed by its realistic roominess for children who share certain developmental deficits. If parents and practitioners are to gain from a case report such as this, the specificity of the child’s symptoms would avoid the uncertainty of a spectrum. The symptoms of the child, M, and their meaning will depict his case as no diagnostic label can do. Lists of his positive and negative symptoms as recorded in a questionnaire completed by his parents before the initial visit are given in Tables 1 and 2. M’s strengths take the lead. Strengths are what leverage healing and provide a novel beginning for a child and his parents whose initial visits with doctors are focused exclusively on their troubles.
Symptoms of this child commonly associated with autism include: silly behavior, sleep disorders such as difficulty falling asleep, early wakening, and awakening screaming, strange poses, shrieking, climbing to high places, destructive behaviors, inconsolable crying, fear of harmless objects, hyperactivity, hand flapping, using adults’ hands to show what he wants, excessive spinning of objects, staring for long periods at blinking lights and fans, staring at his own hands, difficulty stopping movement, frequently holding breath, and talking a few words but only when excited.
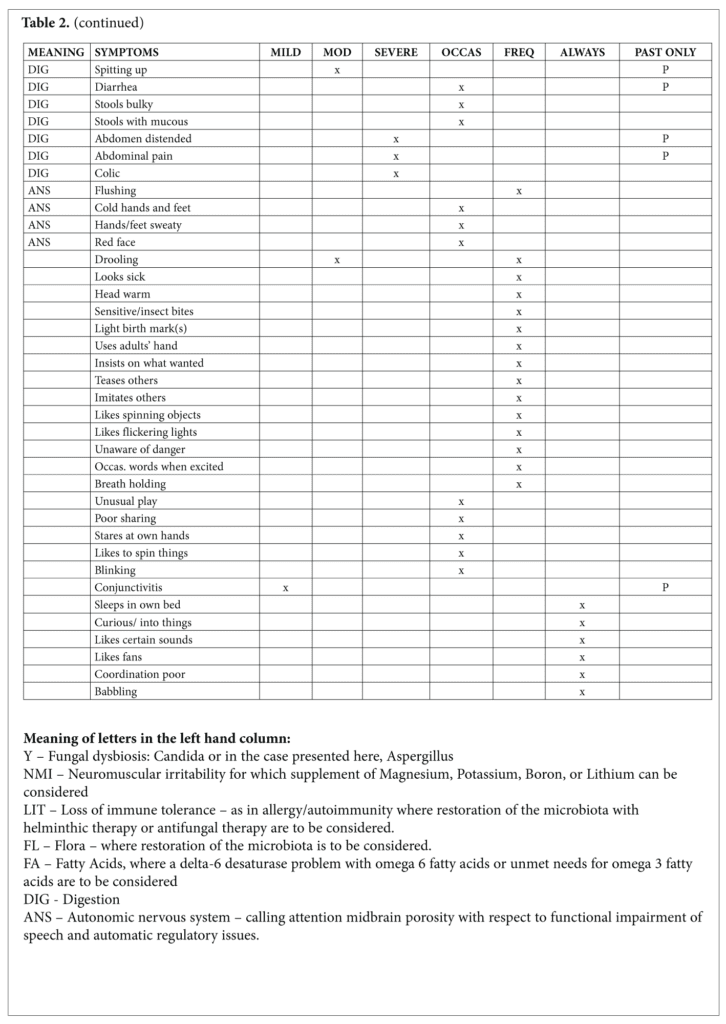
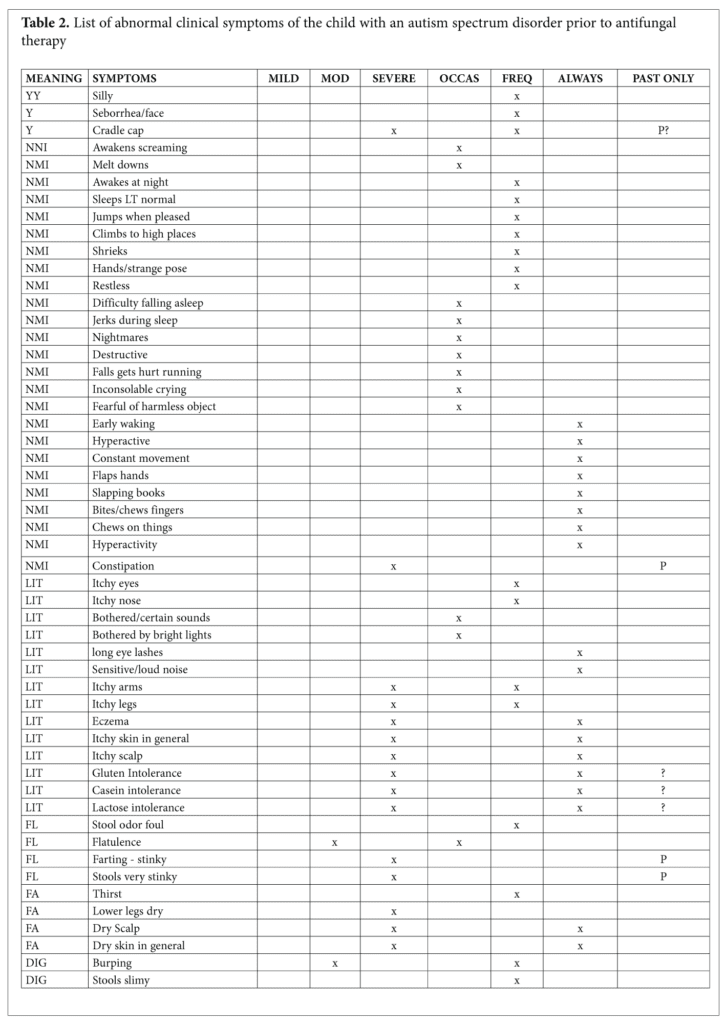
Symptoms of this child that may be associated with dysbiosis or fungal infection include cradle cap, itching of arms and legs, eyes, and nose, constipation, foul-smelling stools, abdominal distension, diarrhea, colic, abdominal pain, and stools that were slimy or had excessive mucus.
A possible connection between mold (fungus) with autism was first proposed by Shaw and his colleagues in 20003 in an open label clinical study of 23 children with autism treated with antifungal therapy using the drug nystatin which is not absorbed from the gastrointestinal tract. In this study, organic acid testing by GC/MS indicated that several compounds associated with Aspergillus species or their metabolic products in humans were significantly elevated in children with autism compared to normal controls. Following antifungal treatment with nystatin for 10 days, there was a significant reduction of the Aspergillus compounds 5-hydroxy-methyl-2-furoic acid, furan-2,5-dicarboxylic acid, and furancarbonylglycine) (Figure 1).
Since nystatin is not absorbed from the gastrointestinal tract, the reduction in these markers of Aspergillus growth after oral nystatin therapy indicated the likely presence of Aspergillus species in the gastrointestinal tract. A recent study4 found high levels of cell-wall deficient (L-forms) filamentous fungi species by culture in nearly all blood samples of children with autism and their mothers. These fungi were not present in normal control blood samples. In addition, the affected children had increased specific IgG, IgM, and IgA serum antibodies to Aspergillus fumigatus. However, antifungal treatment was not attempted in this study.
In another approach to assess the effects of environmental conditions favorable to mold growth on autism prevalence, two studies were conducted to assess autism prevalence with wet environmental conditions favorable for mold growth.5,6 Severity of prenatal exposure to tropical storms and hurricanes, which are frequently associated with water-damaged housing and mold growth, was positively associated with autism prevalence from storm events in Louisiana from 1980 to 1995, especially in mothers who were in mid- or late gestation.5 Precipitation levels were positively correlated with rates of ASD in schools from counties of three western states in the USA.6 A study in 20097 suggested that individual exposure to mold increased the severity of neurophysiological abnormalities seen in autistic children by comparing six autistic children exposed to molds and mycotoxins in the home to eight autistic children with no mycotoxin exposure and 29 non-autistic children, and found that the mycotoxin-exposed autistic group had a 1.8-fold higher number of neurobehavioral abnormalities versus the non-mycotoxin autistic group, and a 12.2-fold higher number of neurobehavioral abnormalities than the non-autistic children.
Materials and Methods
Itraconazole, the generic name of a drug that is considered the standard of care for Aspergillus infections, was used to treat the child. Better results appeared to occur with the brand-name drug Sporanox®. Organic acid testing was performed at The Great Plains Laboratory (now Mosaic Diagnostics), a CLIA certified laboratory that has offered organic acid testing services to physicians for over 20 years using a solvent extraction method, formation of trimethylsilyl derivatives, and gas chromatography-mass spectrometry of the derivatives as described previously.3
Results
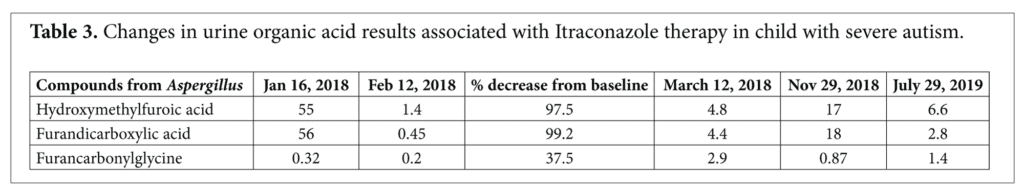
The Aspergillus metabolites 5-hydroxy-methyl-2-furoic acid and furan-2,5-dicarboxylic acid in urine samples of the child with autism decreased 97.5% and 99.2% respectively from the baseline values after antifungal treatment with Itraconazole. Furancarbonylglycine in the urine, which was in the normal range in the baseline sample, decreased 37.5% in the first follow-up sample (Table 3). The first period of antifungal treatment was carried out with incremental increases in dosage after worsening of symptoms. Dr. Baker suspected that the worsening symptoms represented a “die-off ” or Herxheimer response to the release of fungal toxins. M’s family had access to brand name Sporanox® and generic itraconazole. It was only after several weeks of otherwise unexplainable sequences of benefit and negative responses unfolded that a correlation of good responses – including Herxheimer reactions–revealed that the brand name Sporanox® was efficacious and the generic was not. From that point the escalation of dosage produced similar waves of reassuringly similar patterns of exacerbation of negative and breakthrough of positive symptoms. Biweekly measurement of serum AST and ALT reassured us that, even though we were reaching doses that were three-fold the recommended adult dose in this four-year-old boy, the benefits continued to soar. The benefits became realized as he broke through with none of his initial symptoms. Once he stabilized at the maximum dose for a matter of weeks, experimental reductions gave what became a predictable pattern of maintenance of benefit at lower doses until he maintained all of his benefits with no further need for Sporanox® at a time that was a year since the initiation.
All the child’s symptoms of autism had disappeared. In addition, the child developed significant athletic skills in soccer, excellent musical skills, and was assessed at performing at an academic skills level of six years old at the age of four.
Discussion
Aspergillus niger was one of the most common mold/ fungi species in stool samples of normal volunteers along with C. albicans, Penicillium sp., Saccharomyces cerevisiae, and P. herbarum9 but can also result in systemic infection.10-12 Considering that ~0.01% to 0.1% of metagenomic reads from adult stool samples have mapped to fungal species and that fungal genomes are ~3 to 10 times larger than bacterial genomes, it is possible to estimate that of the 1013 microorganisms in the GI tract, about a billion fungal cells compose what is often referred to as the gut mycobiota or mycobiome.9 So the fungal cells represent one ten thousandth of the microbial flora by number in normal people. Many of the A. niger cells in the human intestine are attributed to tree nuts and fruits. There is no simple way to distinguish fungi colonizing the gastrointestinal tract from those that are transient. Strikingly, chronic exposure to low ochratoxin A (OTA) doses could be even more damaging than acute exposure to a high dose and can be produced by A. Niger.12
M’s strengths and symptoms bring precision of individuality to the description of the changes that constituted his cure considering that all his symptoms were alleviated. Considering the parallel changes in his excretion of fungal metabolites, his case is presented as a cure of autism resulting from the reduction of his load of certain toxins. The autism epidemic–along with the increase in prevalence of other chronic illnesses in children – provides strong implications of the role of a wide variety of biogenic, elemental, and synthetic substances in relation to various genetic susceptibilities.13 We have an environment in which children are exposed to a complexity of chemicals and drugs that challenges any effort to assign individual causation.
The lesson of the case we present here is that the child’s microbiota may be the source of toxins that, once identified, will lead to cure with an antimicrobial drug. M’s robust Herxheimer reaction sufficed to provide the expectation that increasing the dose would at some point get us “over the hump” to sustained alleviation of symptoms and an end of the Herxheimer reactions. As it happened, his dramatic benefits persuaded us to increase the daily dose to a peak dose of 600 mg, a dose at which he became free of all his symptoms. At that time, by coincidence, he changed to a new school where developmental testing revealed him – at age 4 – to have the skills of a six-year-old. After sustained improvement for several weeks, his dose was reduced stepwise over a period of six months. He became free of the need for Sporanox® after about 8 months and has remained so and thrived ever since. A particularly touching moment in his recovery came with his offer, before he had been taught to read, at age 6 to read to his parents. He had displayed skills with children’s picture books but his parents were astonished when he read Big Shark Little Shark from beginning to end.
A single child who recovers from autism and a long list of associated symptoms thanks to a treatment with Sporanox® raises what we like to call the coelacanth question. Coelacanth is the name of a primitive fish that was found only as fossils until a live one was caught by a fisherman in the 1930’s. With that catch, no-one suggested that more had to be caught before we could believe coelacanths exist only as fossils. After M’s initial response to Sporanox® and before Dr. Shaw’s laboratory documented Aspergillus as the marker, I began trying a short course of high dose Sporanox® in patients whose history raised the questions of Functional Medicine: “Might this person have an unmet need to get, avoid. or get rid of something that, if taken care of, would favor Nature’s buoyant impulse toward healing. I had learned from my experience with M that there are some sources of generic itraconazole lack efficacy and that a diagnostic trial of Sporanox® is most efficiently done with an increase to 600 mg over a period of seven to ten days.
We cite as an example, a patient whose identical twin’s autism responded to treatments from the protocols of the Defeat Autism Now! consensus document to become a young man with a job. His twin suffered with severe ongoing symptoms that were only partially relieved with antifungal, and a long list of “alternative” and conventional therapies. After Baker’s experience with M, he simply suggested that he take 600 mg of Brand Name itraconazole daily while monitoring his AST, ALT and GGT. His dramatic response surpassed any outcome from all previous treatments including Sporanox® at a normal dose. Shaw reports that he has already found other individuals with autism whose Aspergillus markers are much higher (up to 44 times the upper limit of normal) than the child in this report. In addition, children with autism had very elevated values of one or more of the following mycotoxins when urine samples were tested in Shaw’s laboratory using LC/MS/MS: ochratoxin A, mycophenolic acid, gliotoxin, dihydrocitrinone, roridin E, and enniatin B. In one of these cases of a child with autism with very elevated values of mycotoxins in which house mold testing was done, the testing company stated that inhabitation of the house was not dangerous although some mold was present which should lead to caution when using such services.
A formal trial of itraconazole and Sporanox® for the treatment of autism would seem to be in order. In addition, the finding by Markova4 of filamentous fungi in the serum samples of both children with autism and their mothers suggests additional research to determine possible maternal prenatal transmission of fungi as a cause of autism. Another possible reason for her finding is that both mothers and children were simultaneously exposed to environmental molds.
Authors Disclosure Statement
Shaw is the owner of The Great Plains Laboratory, Inc (now Mosaic Diagnostics), which performs Aspergillus marker testing as part of the organic acid test and mycotoxin tests for physician clients. Neither author has any connection with pharmaceutical companies producing itraconazole or Sporanox®. Patient was seen as an outpatient in Dr. Baker’s office. Biochemical testing was done at The Great Plains Laboratory in Lenexa, Kansas.
References
- Baker SM, Milivojevich A, Kraycar T, Holt B, Gade S. Secular Trend of Sex Ratio and Symptom Patterns Among Children with Autism Spectrum Disorders. Global Adv Health Med. 2014;3(3):92-101. DOI: 10.7453/ gahmj.2014.028.
- Gillberg C. Asperger’s syndrome and recurrent psychosis-a case study. J Autism Dev Disord. 1985;15(4):389-397.
- Shaw W, Kassen E,and Chaves E. Assessment of antifungal drug therapy in autism by measurement of suspected microbial metabolites in urine with gas chromatography-mass spectrometry. Clin Pract Alter Med 2000; 1:15–26.
- Markova, N. Dysbiotic microbiota in autistic children and their mothers: persistence of fungal and bacterial wall-deficient L-form variants in blood. Sci Rep 2019: 9: 13401-13410 https://doi.org/10.1038/s41598-019-49768-9
- Kinney DK, Miller AM, Crowley DJ, Huang E, Gerber E. Autism prevalence following prenatal exposure to hurricanes and tropical storms in Louisiana. J. Autism Dev. Disord. 2008; 38: 481–488.
- Waldman M, Nicholson S, Adilov N, Williams J. Autism prevalence and precipitation rates in California, Oregon, and Washington counties. Arch. Pediatr. Adolesc. Med. 2008; 162: 1026–1034.
- Kilburn KH, Thrasher JD, Immers NB. Do terbutaline- and mold-associated impairments of the brain and lung relate to autism? Toxicol. Ind. Health 2009; 25: 703–710.
- Auchtung TA, Fofanova TY, Stewart CJ, Nash AK, Wong MC, Gesell JR, Auchtung JM, Ajami NJ, Petrosinoa JF. Investigating Colonization of the Healthy Adult Gastrointestinal Tract by Fungi. Msphere 2018;3(2): 1-16 e00092-18
- Bizet J., Cooper C.J., Zuckerman M.J., Torabi A., and Mendoza-Ladd A. A bleeding colonic ulcer from invasive Aspergillus infection in an immunocompromised patient: a case report. Journal of Medical Case Reports 2014; 8:407-412
- Mishra P., Gupta D., Mishra S., and Srinivas V. Aspergillosis of Gastrointestinal Tract Mimicking Malignancy: A Case Report. J Clin Exp Pathol 2017; 7(3):1- 3. doi:10.4172/2161-0681.1000311
- Louthrenoo W, Park YS, Philippe L., and Schumacher H.R. Jr. Localized peripheral calcium oxalate crystal deposition caused by Aspergillus niger. J Rheumatol. 1990;17(3):407-12
- Malir F., Ostry V., Pfohl-Leszkowicz A., Malir J., and Toman J. Ochratoxin A: 50 Years of Research. Toxins 2016; 8:1-49 doi:10.3390/toxins8070191
- Rossignol DA, Genuis SJ, Frye RE. Environmental Toxicants and Autism Spectrum Disorders: A Systematic Review. Transl Psychiatry 2014;4:1-23 e360. doi: 10.1038/tp.2014.4.